Background: Providing health care to rural populations is a major issue in Australia. Disease burden and health risk factors increase with remoteness, but the access to appropriate service decrease. The introduction of Rural Clinical Schools, rural locations for internship and residency, and decentralisation of the Australian General Practitioner Training Program aim to address this disparity. This systematic review aimed at determining if rural placements throughout medical training are associated with future rural general practice in Australia.
Methods: Medline (Ovid), Pubmed, CINAHL and Science Direct were searched for the period January 2000 to July 2019. Included studies related specifically to rural general practitioners in Australia and studies were excluded if they reported only on intention to practice rurally. Evidence was assessed using the Standards for Quality Improvement Reporting Excellence Guidelines.
Results: Eleven articles met the inclusion criteria. Three studies examined the effect of rural placements in medical school on future rural general practice. Three studies looked at placements as a junior doctor on future rural general practice. Four studies looked at the effect of rural general practitioner training on future rural general practice. One study reported on the effect of rural placements during both medical school and junior doctor years on future rural general practice. The studies supported an association between rural placements and future rural general practice, particularly for Australian born doctors, Australian graduates and individuals from rural backgrounds.
Discussion: This review suggests that rural placements during medical training increase the likelihood of future rural general practice. The interplay of personal and professional life influence whether rural intention is sufficient to result in rural practice. Addressing human factors that influence rural practice will contribute to achieving equitable rural health care.
Funding: The authors received no specific funding for this work.
1 Wollongong Hospital, Wollongong, Australia
2 Health Education and Training Institute, NSW, Australia
3 The University of Newcastle, NSW, Australia
Corresponding author: MD, BSc, Alexandra Louise MacDonald, 5 Westmacott Parade, Bulli, New South Wales 2516, Australia, [email protected]
Keywords: rural, general practitioner, training, recruitment, retention
The disparity between health outcomes and access to medical services between urban and rural Australia is an ongoing area of health care concern (AIHW 2017). The 29% of Australians who live outside major cities (AIHW 2017) have higher rates of health risk factors and chronic disease compared to people in major cities (AIHW 2018). Disease burden and age-standardised mortality rates increase with remoteness (AIHW 2017). Rural populations rely more on general practitioner services as a result of reduced access to local specialists (Department of Health 2016). General practitioner supply is maldistributed across different remoteness areas, with the number of general practitioner services provided per capita decreasing with remoteness (AIHW 2019). Therefore, the issue of providing adequate health care to rural and remote populations is a major issue in Australia.
In response to these concerns, rural placement pathways have been introduced into different levels of medical education across Australia in recent decades. These include the introduction of Rural Clinical Schools for university medical students (Eley et al. 2012), providing rural locations for internship and residency (Dunbabin, McEwin & Cameron 2006) and decentralisation of the Australian General Practitioner Training Program (Kitchener 2019). In their 2018 review, O’Sullivan et al. showed that medical school rural immersion programs have a positive effect on rural practice immediately after graduation and in early clinical practice. Parlier et al. (2018) conducted a narrative review of factors involved in recruiting and retaining rural primary care physicians across Australia, Canada and the United States. They identified that rural exposure during medical school and residency contribute towards general practitioners choosing rural practice (Parlier et al. 2018).
This systematic review aims to determine if rural placements in medical school, internship and residency and registrar training are associated with future rural general practice in an Australian context.
A systematic review of the literature was conducted for the period January 2000 to July 2019. The year 2000 was selected as the search start date based on the establishment of the Rural Undergraduate Support and Coordination program in 1997 and the Rural Medical Workforce Strategy in 2001. Terms relating to the effect of rural general practitioner training programs and rural placements during medical training on future rural general practice were searched as keywords (appearing in the title, abstract subject and keyword fields) and mapped against Medical Subject Headings (MeSH) keywords (Appendix 1). The electronic databases used were Medline (Ovid), Pubmed, CINAHL and Science Direct. Bibliographies of relevant articles were also hand searched.
Papers identified in database searches were exported to Rayyan for screening. Duplicates were removed, then title and abstract screening against inclusion criteria was conducted by one reviewer (AM). Full text screening was completed independently by two reviewers (AM, KD), with conflicts resolved by consensus. Studies were included in this review if they met the following criteria: related specifically to the recruitment or retention of general practitioners, presented findings from primary research, were from Australian data and were available in English. Qualitative and quantitative studies were included. Studies were excluded if they reported on participants’ intention to practice rurally rather than providing data on actual rural general practice.
The included studies were summarised using a piloted and revised data extraction form, including a combination of the following items: study design, data type, sample size, population, placement type and results. The strength of evidence for each of the studies included for review was assessed using the Standards for Quality Improvement Reporting Excellence Guidelines (Ogrinc et al. 2016) (Appendix 2).
Study characteristics and critical appraisal outcomes were collated for comparative purposes (see Table 1). Quantitative results and qualitative findings concerning the effects of rural placements on recruitment and retention of rural general practitioners were grouped according to the timing of rural placement during medical training. The methods and reporting in this systematic review were completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al. 2009) (Appendix 3).
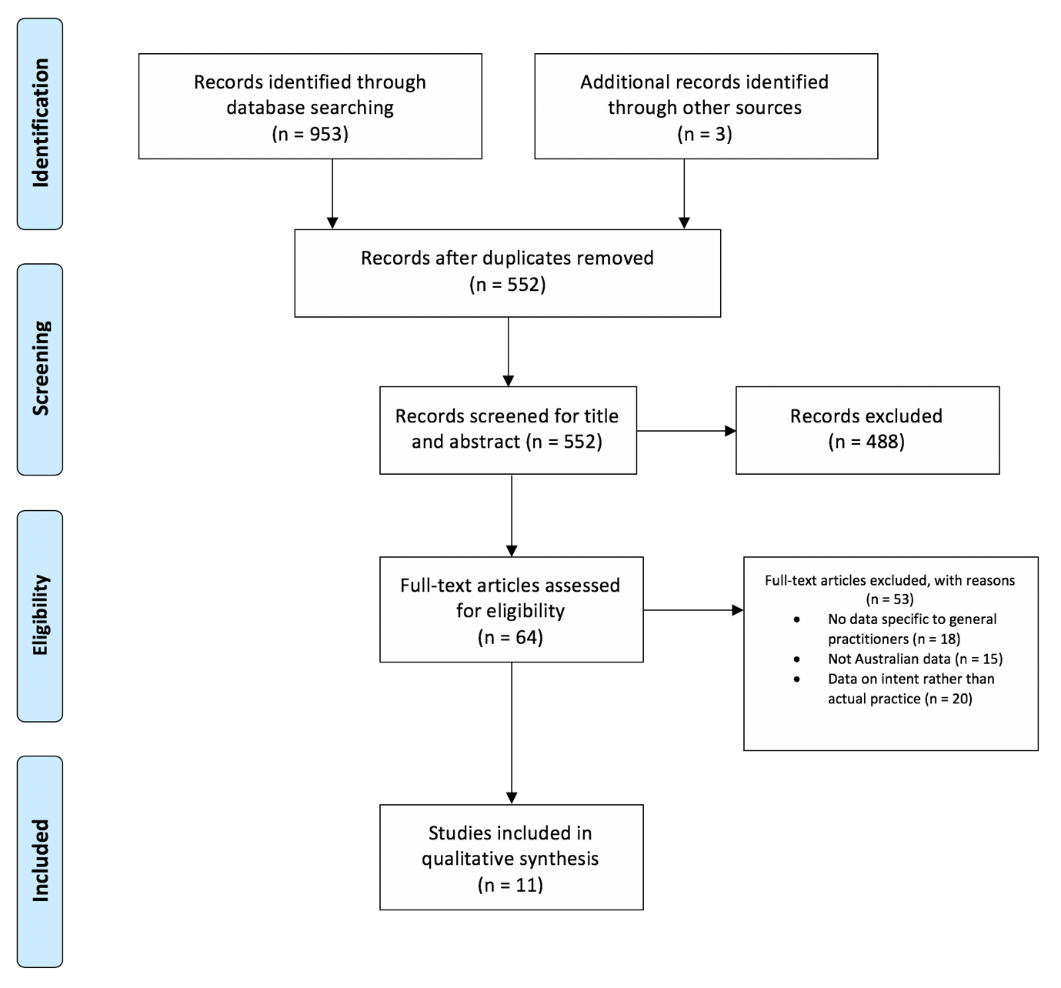
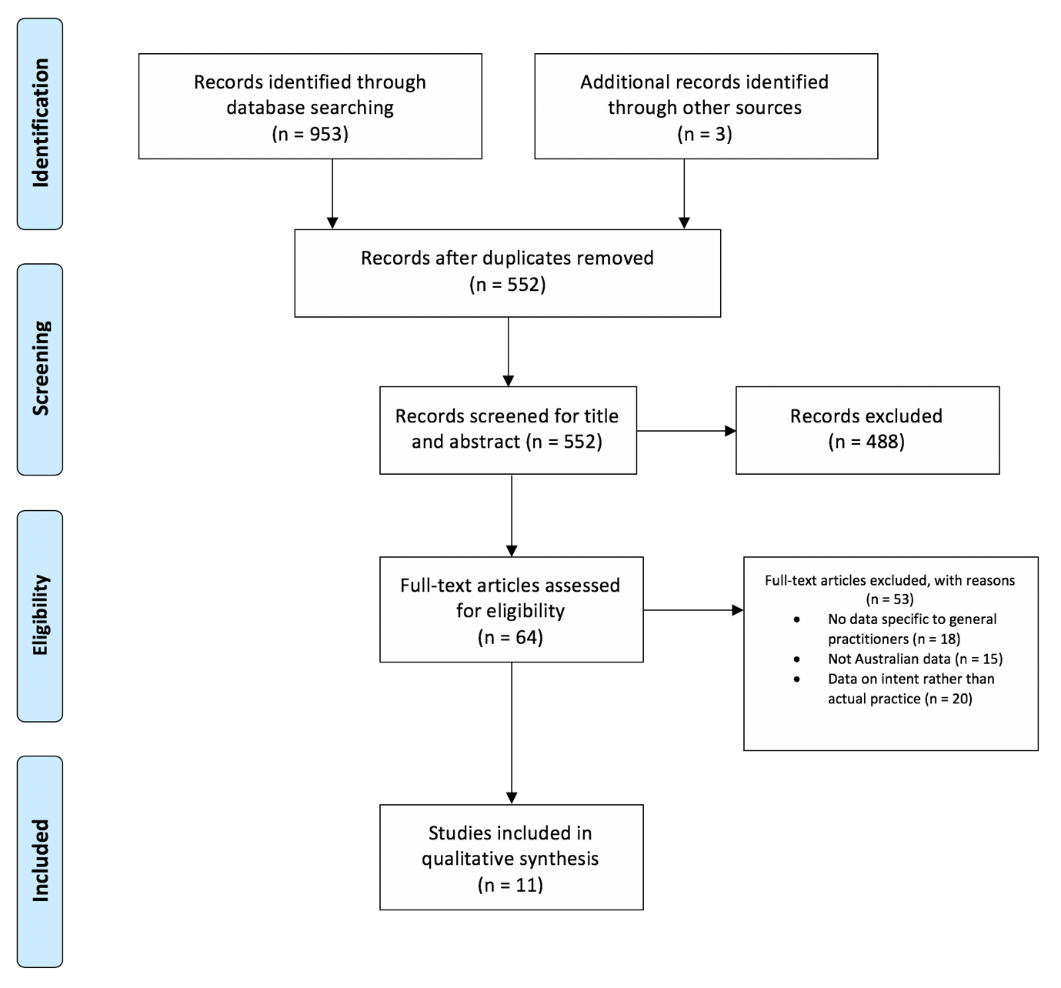
The electronic database search identified a total of 953 studies (see Figure 1). Three additional articles were identified while hand-searching bibliographies. Of these studies, 404 duplicates were removed, leaving 552 studies for screening title and abstract. Four hundred and eighty-eight studies were excluded based on title and abstract, resulting in 64 studies for full text assessment. A total of 11 articles remained that met the inclusion criteria of this review (Eley et al. 2012; Dunbabin, McEwin & Cameron 2006; Kitchener 2019; Kwan et al. 2017; Playford, Ng & Burkitt 2016; Wilkinson et al. 2003; Lewis et al. 2016; Peach, Trembath & Fensling 2004; McGrail, Russell & Campbell 2016; Robinson & Slaney 2013; Wearne et al. 2010).
Studies were grouped according to the time in training at which the rural placement occurred. Three studies examined the effect of rural placements in medical school on future rural general practice (Eley et al. 2012; Kwan et al. 2017; Playford, Ng & Burkitt 2016). Three studies looked at placements as a junior doctor on future rural general practice (Dunbabin, McEwin & Cameron 2006; Lewis et al. 2016; Peach, Trembath & Fensling 2004). Four studies looked at the effect of rural general practitioner training on future rural general practice (Kitchener 2019; McGrail, Russell & Campbell 2016; Robinson & Slaney 2013; Wearne et al. 2010). One study reported on the effect of rural placements during both medical school and during junior doctor years on future rural general practice (Wilkinson et al. 2003). The study characteristics and findings of these studies are summarised in Table 1. The studies were assessed using the Standards for Quality Improvement Reporting Excellence Guidelines (Ogrinc et al. 2016), and, overall, they partially achieved the guidelines, indicating low to moderate study quality (Appendix 2).
|
Study |
Study Type |
Population |
Placement Type |
Results |
|---|---|---|---|---|
|
Eley et al. (2012) |
Longitudinal mixed methods |
UQ RCS |
Medical School |
40% working outside major city GP most frequent specialty choice (24%) Encouraged 70% of students towards rural medicine |
|
Dunbabin et al. (2006) |
Survey |
NSW RMO Cadetship |
Internship/Residency |
43% working rurally
Practice location influenced career choice |
|
Kitchener et al. (2019) |
Operational audit |
AGPT QLD |
GP Training |
55% Practising in rural locations Significant (p<0.01) increase in retention compared to before AGPT program(OR = 2.1; 95%CI [1.2-3.7]) |
|
Kwan et al. (2017) |
Cross sectional cohort |
UQ RCS |
Medical School |
Independent and duration dependent predictor of rural GP Additive effect of rural background |
|
Playford et al. (2016) |
Survey |
UWA RCS |
Medical School |
17% practising rurally Majority general practitioners Equivalent for urban and rural origin alumni |
|
Wilkinson et al. (2003) |
Case-control |
National GP database |
Medical school and internship/residency |
Rural GPs more likely to report rural medical school training (OR = 1.61; 95%CI [1.32-1.95]) and rural internship/residency training {OR = 3.14; 95%CI [2.57-3.83]) Increased duration increased likelihood of GP |
|
Lewis et al. (2016) |
Survey |
NSW RMO Cadetship |
Internship/Residency |
GP most popular specialty choice (43%) 53% practising rurally Practice location influenced career choice (p <0.01) 44% indicated cadetship influenced decision |
|
Peach, Trembath & Fensling (2004) |
Retrospective follow-up |
Ballarat Base Hospital Interns |
Internship/Residency |
BBH interns more likely to be practising as GPs in non-metropolitan areas than were interns from metropolitan hospitals (p<0.01, 95% CI [17%-45%]) |
|
McGrail, Russell & Campbell (2016) |
Cohort |
Nationwide |
GP Training |
Rural training pathway significantly associated with subsequent rural practice Odds of rural practice decreased with time, but retained across the five years |
|
Robinson & Slaney (2013) |
Survey |
Bogong GP Registrars |
GP Training |
42% in rural practice, 32% in Bogong region Significant relationship between country of birth and remaining in rural practice (χ2 = 13.68, p<0.01) |
|
Wearne et al. (2010) |
Survey |
Remote Training Graduates |
GP Training |
81% currently working RRMA3 or above 47% currently working RRMA4 or above 41% currently working RRMA5 or above 20% currently working RRMA6 or above |
Four studies reported on the effect of rural placements during medical school on future rural general practice (Eley et al. 2012; Kwan et al. 2017; Playford, Ng & Burkitt 2016; Wilkinson et al. 2003). Study types included a longitudinal cohort study (Playford, Ng & Burkitt 2016), a longitudinal mixed-methods sequential exploratory design (Eley et al. 2012), a cross-sectional cohort study (Kwan et al. 2017) and a case-control study (Wilkinson et al. 2003). Overall, the studies supported an association between rural placements during university and future practice as a rural general practitioner. Two of these studies included a control group with which to compare rates of rural general practice (Kwan et al. 2017; Wilkinson et al. 2003). Kwan et al. (2017) reported that attendance at a rural clinical school (RCS) to be an additive predictor of future rural general practice, with higher odds of rural practice after one year (OR = 2.85; 95% CI [1.77–4.58]) and two years (OR = 5.38; 95% CI [3.15–9.20]) compared to those attending a metropolitan clinical school, independent of whether students had a rural background. The highest association between rural training and rural practice was 84% for general practitioners who had both a rural background and two years attending an RCS (Kwan et al. 2017). Wilkinson et al. (2003) found rural general practitioners were more likely to report rural placements during university (OR = 1.61; 95% CI [1.32–1.95]) than urban general practitioners.
Survey data from RCS graduates was reported in two studies that did not include a control group. Seventeen per cent of RCS graduates from Western Australia (Playford, Ng & Burkitt 2016) and 40% of RCS graduates from Queensland (Eley et al. 2012) were practising rurally, and general practice was the most commonly reported specialty (Eley et al. 2012; Playford, Ng & Burkitt 2016). Follow-up interviews with 29 participants revealed that rural experience in the RCS was a primary driver of influence on early career decisions but was often overridden by personal and family motivators (Eley et al. 2012). New graduates and doctors in training are in an age range where they are commonly confronted with major life decisions (Eley et al. 2012), and these affect career decisions.
Four studies reported on the effect of rural placements during internship and residency (Dunbabin, McEwin & Cameron 2006; Wilkinson et al. 2003; Lewis et al. 2016; Peach, Trembath & Fensling 2004). Study types included a case-control (Wilkinson et al. 2003), retrospective follow-up (Peach, Trembath & Fensling 2004) and two surveys (Dunbabin, McEwin & Cameron 2006; Lewis et al. 2016). Although only two out of the four studies presented control group data (Wilkinson et al. 2003; Peach, Trembath & Fensling 2004), overall rates of rural general practice were promising. In a retrospective follow-up, 44% of rural interns had continued to become general practitioners outside metropolitan areas compared to 13% of metropolitan interns (difference, 31%; 95% CI [17%–45%]; p < 0.001) (Peach, Trembath & Fensling 2004). Rural general practitioners were more likely to report having rural training as junior doctors (OR 3.14; 95% CI [2.57–3.83]), with the likelihood of working as a rural general practitioner increasing with time spent rurally during training (OR 10.52; 95% CI [5.39–20.51]) (Wilkinson et al. 2003).
Two studies reported on data from the Rural Resident Medical Officer Cadetship Program (Dunbabin, McEwin & Cameron 2006; Lewis et al. 2016). When cadets were followed up in these studies, 42% (Dunbabin, McEwin & Cameron 2006) to 53% (Lewis et al. 2016) of cadets were working in a rural area. The most common choice of vocational training was general practice (Lewis et al. 2016), and 58% of those practising rurally were general practitioners (Dunbabin, McEwin & Cameron 2006).
A notable finding in two studies was the effect of practice location on career choice, with those practising rurally tending towards general practice than other specialties, p < 0.001 (Dunbabin, McEwin & Cameron 2006; Wilkinson et al. 2003).
Four studies reported on the effect of rural placements during general practitioner registrar training on future rural practice (Kitchener 2019; McGrail, Russell & Campbell 2016; Robinson & Slaney 2013; Wearne et al. 2010). Studies included two surveys (Robinson & Slaney 2013; Wearne et al. 2010), an operational audit (Kitchener 2019) and a cohort study that compared the retention rates of rural training registrars to metropolitan trainees (McGrail, Russell & Campbell 2016). They reported that 74–91% of rural training/rural origin and 87–95% of metropolitan training/metropolitan origin groups remained in their location type for the five years post-training (McGrail, Russell & Campbell 2016). The cohorts with mixed geographical combinations (rural training/metropolitan origin and metropolitan training/rural origin) tended to remain in the training location type initially and gradually move towards their origin type over the following years (McGrail, Russell & Campbell 2016). Rural general practitioner training was significantly associated with future rural practice when compared to metropolitan training for both rural origin (OR 159; 95% CI, 45–558, p < 0.05;) and metropolitan origin (OR 68; 95% CI, 26–175, p < 0.05) groups (McGrail, Russell & Campbell 2016). This effect decreased with time but remained significant (McGrail, Russell & Campbell 2016).
The remaining studies presented rates of retention from rural trainees only. Results ranged from 42% (Robinson & Slaney 2013) to 55% (Kitchener 2019) retained in rural general practice. Thirty-two per cent remained in their area of rural training (Robinson & Slaney 2013). Australian medical program graduates were more likely to be practising rurally than international graduates (Kitchener 2019), and Australian born doctors were more likely to be practising rurally than overseas-born doctors (χ2 = 13.68, p < 0.001) (Robinson & Slaney 2013). Wearne et al. (2010) presented retention rates for different categories or rurality. Overall retention rates were 81% in RRMA 3 or above, 47% in RRMA 4 or above, 41% in RRMA 5 or above, 20% in RRMA 6 or above and 16% in RRMA 7 (Wearne et al. 2010). Participants in this study all felt that the Remote Vocational Training Scheme had prepared them to some degree for rural practice (Wearne et al. 2010).
The results of this systematic review indicate that there is preliminary evidence that exposure to rural placements during medical training is associated with future rural general practice. This finding was consistent across rural placements while at university, during internship and residency and during registrar training. Australian born doctors and Australian medical graduates were reported as being more likely to be rural general practitioners following rural placements than overseas-born or international medical graduates (Kitchener 2019; McGrail, Russell & Campbell 2016; Robinson & Slaney 2013). The effect of rural placements also appears to be enhanced by an individual or their spouse or partner being of rural background (Lewis et al. 2016; McGrail, Russell & Campbell 2016; Robinson & Slaney 2013). Other life decisions that were reported to substantially affect practice location were opportunities for children and proximity to family. These factors may prevent doctors who intended on practising as rural general practitioners from being able to do so (Eley et al. 2012; Robinson & Slaney 2013).
This review lends further evidence in support of the pipeline metaphor (Murray & Wronski 2006), which suggests a sequence of rurally orientated programs linking the stages of medical training from medical school through to completion of specialist training and beyond. Provision of training opportunities also contributed towards a tendency toward rural general practice (Eley et al. 2012; Dunbabin, McEwin & Cameron 2006; Wilkinson et al. 2003; Robinson & Slaney 2013) and this tendency was further amplified among those of rural origin (Kwan et al. 2017; Wilkinson et al. 2003; Lewis et al. 2016; McGrail, Russell & Campbell 2016). The results of this study are consistent with those of a 2018 review (O’Sullivan et al. 2018), which also suggested rural immersion during medical school was associated with rural practice in career but lacked control data. Our findings also align with a multidimensional theoretical model of rural primary care physician recruitment that includes rural background, rural exposure, training opportunities and family receptivity to a rural location (Parlier et al. 2018).
Further research involving nationally delivered programs and randomisation of participants to control, as well as rural training groups, would be beneficial to inform policy decisions, but this is unlikely to be feasible. Given the different levels of training in which rural placements can be undertaken, it would also be beneficial to investigate which of these individually and in combination have the greatest effect on rural retention. The issues commonly raised in qualitative analysis, such as family and the effect of personal factors on rural practice, would also benefit from undergoing quantitative exploration with larger participants so that targeted approaches can be introduced and assessed. It would also be interesting to investigate whether rurally trained doctors are more likely to move to rural localities to practice later in their careers when family circumstances may have changed.
While this review indicates that rural placements during medical training increase the likelihood of future rural general practice, there were limitations to the review and included studies.
The majority of the studies were observational and lacked a control group. This limitation was reflected in the low to moderate study quality ratings of included studies. As a result, it is difficult to determine if the reported rates of rural practice are due to rural placement during training or other contributing factors. Included studies were susceptible to self-selection bias, as participants who chose rural placements may be more likely to practice rurally regardless of exposure during training. Methodological rigour could be increased in future studies by controlling for known confounders so that the effect of rural placements can be isolated.
While the methods and reporting of this systematic review adhered to the PRISMA guidelines, the generalisability of findings beyond Australia are somewhat limited due to country-specific training pathways. Due to study heterogeneity, it was not possible to further consolidate results or conduct meta-analyses.
Rural placements during medical training increase the likelihood of future rural general practice. The issue of sustaining a rural general practice workforce is complex. Positive experiences and intentions from rural placements can be outweighed by personal and professional factors that thwart intentions for future rural practice. Rural general practice is vital to improving health service delivery in underserved rural and remote populations. A model for incorporating rural placements in all stages of medical training could improve rural general practitioner recruitment and retention and redress this imbalance.
The authors have no conflicts of interest to declare
Australian Institute of Health and Welfare (AIHW) 2019, Rural & remote health
Australian Institute of Health and Welfare 2017, Australia’s welfare 2017, AIHW, Canberra
Australian Institute of Health and Welfare 2018, Australia’s health 2018, AIHW, Canberra,