
Introduction: MASK-EDTM simulation is a novel educational approach in which a clinically experienced educator dons a high-fidelity silicone mask and plays the role of a patient. MASK-EDTM simulation has not yet been evaluated in physiotherapy education. The purpose of this study was to describe physiotherapy students’ perceptions of the value of MASK-EDTM simulation and its effect on perceived preparedness for clinical placements.
Methods: Design: Mixed-methods cohort study, using questionnaires and focus groups over 12 months.
Setting: Entry-level Physiotherapy course at an Australian university.
Participants: Eighty-one physiotherapy students enrolled in their first unit of cardiorespiratory Physiotherapy.
Intervention: MASK-EDTM simulation in five tutorials across two semesters, practising skills including history-taking and secretion clearance techniques.
Main outcome measures: Questionnaires pre- and post clinical placement; thematic analysis of focus group data following clinical placement exposure.
Results: One hundred per cent of students described MASK-EDTM as helpful in developing manual handling skills (mean 3.8/4.0, SD 0.4), establishing rapport and empathy with patients (mean 3.7/4.0, SD 0.5), and communicating with an older patient (mean 3.4/4.0, SD 0.6). Following exposure to clinical placement, students perceived MASK-EDTM as slightly less helpful in enhancing readiness for clinical placement (MD –0.20 out of 5, 95% CI -0.54 to –0.04) compared with before clinical exposure. However, they still considered MASK-EDTM somewhat helpful (mean 3.2/4.0). Three themes were identified: the safety of the learning environment with MASK-EDTM, the importance of communication in MASK-EDTM simulation and the performative aspects of MASK-EDTM simulation. All three themes were underpinned by the importance of authenticity in learning and practice.
Conclusions: Physiotherapy students perceive MASK-EDTM simulation asvaluable in enhancing learning relating to clinical practice, particularly prior to clinical placement.
Keywords: education, simulation, physiotherapy (techniques)
1University of Canberra, Bruce ACT, Australia
Corresponding author: Associate Professor Bernie Bissett, Physiotherapy, University of Canberra,Bruce ACT, 2617 Australia. [email protected]
Like many health students, physiotherapy students must learn a wide range of skills for effective clinical practice. The clinical skills required in physiotherapy are extensive and include a range of communication strategies, clinical reasoning skills, manual techniques and exercise strategies. Simulation is an effective approach for enhancing learning across health professions (Barsuk et al. 2009; Fraser et al. 2009; Sturm et al. 2008).
Simulation often mimics the clinical environment and can encompass various activities, from role play to interactive computer games to high-fidelity mannequins (Jeffries 2005). MASK-EDTM is a novel simulation technique where expert clinicians don a high-fidelity silicone mask to play the role of an older patient, allowing students to interact with a life-like older ‘patient’ (Reid-Searl et al. 2011; Reid-Searl et al. 2012). MASK-EDTM simulation allows the experienced clinician beneath the mask to steer the interaction with the student, capitalising on spontaneous teaching moments and then debriefing with the student afterwards (McAllister, Levett-Jones et al. 2013).
The perception of MASK-EDTMT simulation has been evaluated in nursing students, appearing to increase confidence and preparedness for clinical practice while decreasing anxiety (Reid-Searl et al. 2012). Kable et al. (2013) compared MASK-EDTM with simulation using live actors and high-fidelity mannequins in nursing students. They found that students perceived MASK-EDTMT to be more effective for learning and preparedness for clinical practice and significantly more authentic in relation to clinicalpractice than other forms of simulation. However, the utility of MASK-EDTM in physiotherapy has not yet been evaluated.
In our university, we have five years’ experience using MASK-EDTM. ‘Joyce’, our MASK-EDTMT character, is a 76-year-old lady with pulmonary fibrosis (Figure 1). Joyce has a carefully curated past medical history, including hypertension, osteoporosis and arthritis, as well as a realistic social history. In line with MASK-EDTM methodology, each component of Joyce’s story is linked with the cardiorespiratory physiotherapy unit’s learning objectives (Reid-Searl et al. 2011). Importantly, the educator behind the mask has more than 15 years’ experience working in the hospital setting as a cardiorespiratory physiotherapist and over 10 years’ experience in clinical education. Thus, the educator can steer interactions with physiotherapy students and prompt spontaneous and relevant learning more readily than a trained actor. Although student surveys have indicated that students enjoy MASK-EDTM (unpublished data), we have not yet ascertained which specific aspects of skill development students perceive to be enhanced by this form of simulation. We have also not yet explored the relationship between classroom MASK-EDTM exposure and perceived readiness for clinical placement.

Therefore, this study aimed to explore students’ perceptions of the experience of MASK-EDTM in a physiotherapy classroom context, including perceptions of whether MASK-EDTM enhanced specific aspects of learning. Further, we sought to ascertain whether MASK-EDTM affects students’ perceptions of readiness for clinical placement, particularly in a hospital-based setting where students encounter many older patients.
A mixed-methods cohort study design was used to collect quantitative data using rating scales within questionnaires and qualitative data through focus groups. Mixed-methods research allows the research question to be answered through both quantitative and qualitative data (Creswell 2009). A qualitative descriptive approach underpinned the study (Braun & Clarke 2008; Cooper & Endacott 2007).
Participants were recruited from students enrolled in a four-year undergraduate physiotherapy program and a two-year graduate-entry physiotherapy program. These students had no previous exposure to MASK-EDTM simulation or other forms of simulation or clinical placement. All students enrolled in their first cardiorespiratory physiotherapy unit of study were invited to participate. Students wereapproached at the end of a tutorial and given verbal and written information about the study. Subsequently, all students who completed a hospital-based placement were invited to participate in the focus groups. The study was conducted in accordance with the university’s human research ethics committee, and all participants provided written informed consent.
This study was undertaken in an Australian university. Participants were enrolled in their first cardiorespiratory physiotherapy unit of study, which primarily addresses the physiotherapy assessment and treatment of basic medical and surgical conditions. There is a strong emphasis on practical skills such as mobilising patients with multiple attachments (i.e., drips and drains) following surgery, and secretion clearance techniques such as postural drainage, percussion and positive expiratory pressure therapy. This unit of study occurs prior to any clinical placements. Students are required to complete five different clinical placements during the degree, not all of which are hospital based (i.e., some occur in community settings, such as private practice). Allocation to these clinical placements is dependent on availability, and not all students have a hospital-based placement at the same time. As such, only a proportion of students complete a hospital-based clinical placement immediately after the cardiorespiratory physiotherapy unit of study.
Students were exposed to the MASK-EDTM character Joyce during five tutorials (three tutorials in Semester 2 2015 and two tutorials in Semester 1 of 2016), resulting in five separate simulation scenarios (Table 1). Students were provided with the relevant medical history, observations and medical reports, as well as Joyce’s most recent physiotherapy assessment findings. In groups of four, students had the opportunity to either treat Joyce directly or play the supervisors’ role. Students had 10 minutes in which to provide treatment. Each tutorial also included group debriefing, reflection and peer feedback after the simulation scenario.
|
Exposure to MASK-EDTM simulation |
Simulation scenario |
|---|---|
|
Exposure 1 |
Joyce arrived in the classroom to meet the students, ostensibly to give them the opportunity to ask questions about her health. The students were exposed to the challenging tangential nature of history-taking with a talkative patient who likes to ask questions of their own. |
|
Exposure 2 |
Students encountered Joyce in a mock hospital ward scenario, where she had been admitted with community-acquired pneumonia, on a background of pulmonary fibrosis. Students were required to implement an evidence-based intervention for Joyce. |
|
Exposure 3 |
Students encountered Joyce in another mock hospital ward scenario, where she had undergone major abdominal surgery. Students were required to implement an evidence-based intervention for Joyce. |
|
Exposure 4 |
Joyce arrived in the classroom as the students were learning how to implement a respiratory questionnaire (the Chronic Respiratory Disease Questionnaire), so they practised with Joyce. |
|
Exposure 5 |
Joyce arrived in the classroom as the students were learning motivational interviewing skills, and she agreed to be interviewed in front of the class by the classroom tutor. |
The first questionnaire was completed by all participants at the end of a tutorial, following their third exposure to MASK-EDTM simulation. The second questionnaire was completed only by students who had completed their first hospital-based clinical placement (Figure 2b). This was also completed at the end of a tutorial. The questionnaires were distributed and collected by a researcher who was not involved in teaching the cardiorespiratory unit or in the provision of MASK-EDTM simulation to reduce bias. Students who did not want to participate were allowed to leave the room. The first questionnaire aimed to determine participants’ perception of MASK-EDTM simulation in relation to in-class learning before participating in any clinical placements. This questionnaire contained 15 items rated from 0-4 (0 = ‘very unhelpful’ and 4 = ‘very helpful’). The second questionnaire aimed to determine participants’ perception of MASK-EDTM simulation in preparing them for a hospital-based clinical placement; it was collected after they had completed a hospital-based clinical placement. The eight items relating to clinical skills were repeated in both questionnaires (Figure 2a).
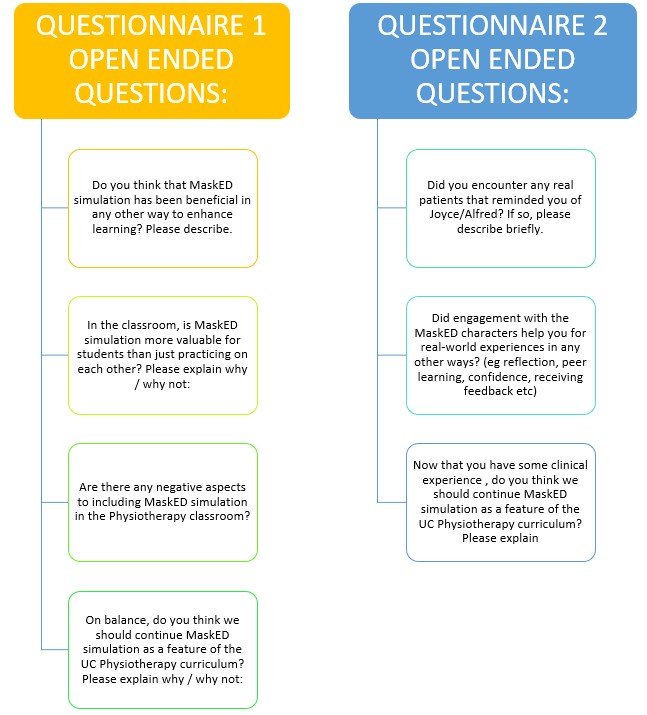
All students who completed a hospital-based clinical placement were invited to participate in the focus groups. Focus groups aimed to include 10 students and were conducted at the university within a month of students completing their clinical placement. They were facilitated by a researcher who was experienced in running focus groups and involved in teaching some physiotherapy units. Focus groups were audio-recorded for transcription. Students were asked open-ended, predetermined questions (Figure 3) developed based on responses to the first two questionnaires and previous literature on MASK-EDTM(Kable et al. 2013; McAllister, Levett-Jones et al. 2013; Reid-Searl et al. 2011; Reid-Searl et al. 2012).

Quantitative and qualitative data were analysed separately. Quantitative data are presented as mean (SD) and 95% confidence intervals. The focus group discussions were professionally transcribed verbatim and checked for accuracy by the focus group facilitator to minimise bias. The transcripts were then analysed thematically using an inductive approach. Two research team members independently read and listened to all audio-recorded qualitative data and coded the transcripts, identifying potential themes. A further phase of defining and analysing themes was undertaken, including establishing a coherent thematic map that was retested against original data extracts (Braun & Clarke 2008). These final themes were then discussed and verified by all researchers until consensus was reached.
Eighty-one students were invited to participate in the study, and all initially consented to participate (Figure 4). All 81 students completed the first questionnaire, and 48 students (all those who had completed a hospital-based clinical placement) completed the second questionnaire. In total, 35 students took part in four focus groups.
Quantitative results are presented in Table 2. One hundred per cent of students described MASK-EDTM as helpful in improving their ability to apply theory to practice, engage with the material covered in the unit, remember practical aspects of the lesson, prepare for practical exams, self-reflect and learn from mistakes in a safe environment, receive effective feedback and utilise peer learning.
|
Criteria (0–4) 0 = very unhelpful 4 = very helpful |
Score before clinical placement, Mean (SD) (n = 81) |
Score after clinical placement, Mean (SD) (n = 48) |
Difference between scores (after clinical minus before clinical), Mean (95% CI) (n = 48) |
p value |
|---|---|---|---|---|
|
Interest/engagement with the material covered in the unit |
3.59 (0.61) |
|
||
|
Ability to apply theory to practice |
3.66 (0.57) |
|||
|
Self-reflection and learning from mistakes in a safe environment |
3.80 (0.43) |
|||
|
Potential to learn from other students’ experiences (peer learning) |
3.66 (0.57) |
|||
|
Ability to give/receive feedback |
3.55 (0.59) |
|||
|
Readiness to undertake the practical exam |
3.55 (0.61) |
|||
|
Remembering practical lessons from the classroom |
3.65 (0.57) |
|||
|
Confidence engaging with an older person |
3.52 (0.55) |
3.40 (0.64) |
–0.13 (–.36 to 0.12) |
0.391 |
|
Developing rapport and empathy with patients |
3.71 (0.50) |
3.47 (0.58) |
–0.24 (–0.46 to –0.02) |
0.029* |
|
Manual handling skills |
3.85 (0.41) |
2.69 (0.80) |
–0.17 (1.42 to 0.9) |
0.000* |
|
Management of attachments in a realistic scenario |
3.81 (0.39) |
3.27 (0.82) |
–0.54 (–0.80 to –0.28) |
0.000* |
|
Communicating with an older patient |
3.44 (0.62) |
3.31 (0.55) |
–0.13 (–0.37 to 0.11) |
0.228 |
|
Explaining treatments without using jargon |
3.52 (0.62) |
3.46 (0.62) |
–0.06 (–0.31 to 0.19) |
0.574 |
|
Ability to step into the physio role |
3.79 (0.46) |
3.08 (0.85) |
–0.71 (–0.99 to –0.43) |
0.000* |
|
Readiness to undertake clinical placement |
3.46 (0.62) |
3.17 (0.63) |
–0.29 (–0.54 to –0.04) |
0.021* |
One hundred per cent of students perceived that MASK-EDTM was helpful for clinical skills. This included increasing their confidence in engaging with an older person; developing rapport, empathy and communication skills; implementing manual handling skills; managing attachments (e.g., drips and drains in a post-surgical patient); and a sense of preparedness for their physiotherapist role in a clinical placement setting. Students perceived MASK-EDTM to be most helpful in developing manual handling skills (mean = 3.85/4.0). Students also reported that MASK-EDTM was somewhat helpful in developing their self-perceived readiness for clinical placement (mean = 3.5/4.0).
Relative to pre-placement ratings, there was a significant decrease in students’ perception of the ability of MASK-EDTM simulation to develop rapport and empathy with patients (MD -0.24 out of 4, 95% CI -0.46 to -0.02), manual handling skills (MD -1.16 out of 4, 95% CI -1.42 to -0.9), management of attachments in a realistic scenario (MD -0.54 out of 4, 95% CI -0.80 to -0.28), the ability to step into the physio role (MD -0.71 out of 4, 95% CI -0.99 to -0.43) and readiness to undertake clinical placement (MD -0.20 out of 4, 95% CI -0.54 to -0.04). There was no difference in students’ pre- and post-clinical placement perception of the ability of MASK-EDTM simulation to contribute to confidence in engaging with older persons, communicating with older patients and explaining treatments without using jargon.
Analysis of the qualitative data from the focus groups resulted in the identification of three distinct themes: 1) the safety of the learning environment; 2) the importance of communication skills; and 3) the performative aspect of the simulation experience. These three themes were all underpinned by the concept of authenticity (Figure 5) and each will be explored through that lens.
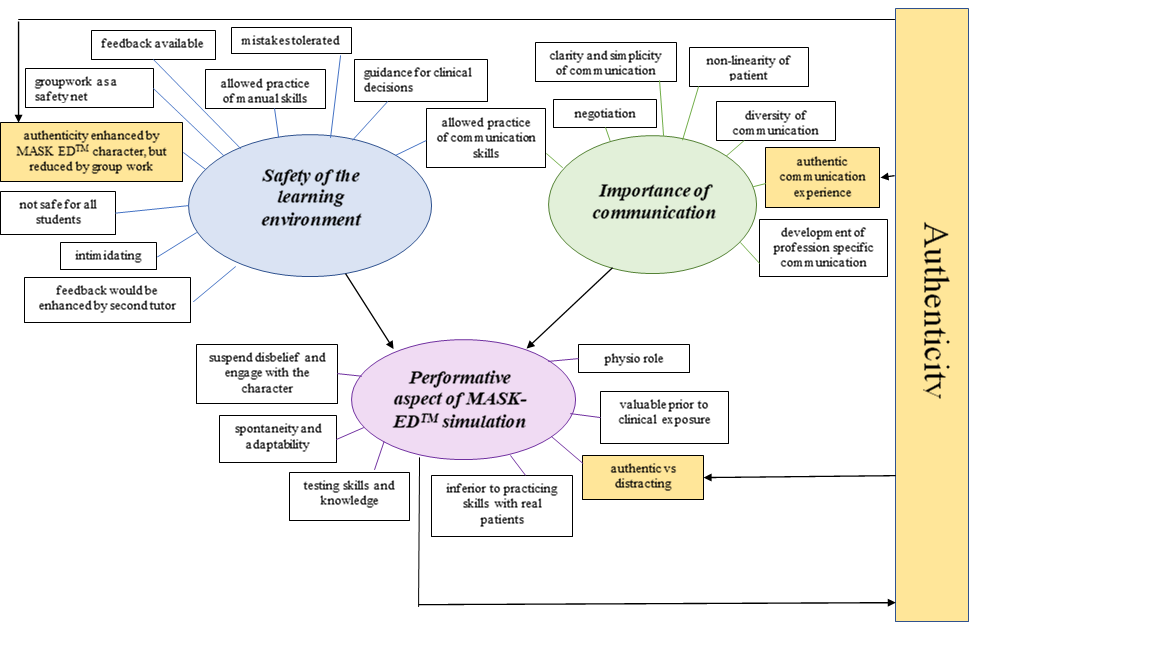
Many students perceived that the learning environment was enhanced by MASK-EDTM simulation because it allowed skill learning to be undertaken in a safe environment (where mistakes would be tolerated) and feedback would be readily available to guide clinical decisions. Skill acquisition in this safe learning environment encompassed both manual skills (e.g., physical handling of the patient) and communication skills. The presence of an expert guiding the MASK-EDTM simulation was regarded as highly valuable by many students, particularly as they could ensure the safety of that learning experience:
‘Very useful that the person wearing the mask knows what is going on and can guide the situation appropriately’.
‘And if you put the mask on it makes it not [the lecturer] we’re talking to, but also not an actual old person, so if we do say something stupid … your lecturer goes “don’t say that” [laughs] You’re not offending anyone’.
Further, some students identified that authenticity of the MASK-EDTM character could be achieved safely in the learning environment and that this was inherently different from practising with their peers:
‘Good to build confidence in a safe, non-confronting environment with no pressure’.
‘It was really good to practice communicating, because just having the mask on I’d forget it was [lecturer], you’d think it was a whole different person’.
‘It’s very different practising with a friend to actually practising with a realistic patient. It’s nice, she’s more realistic than talking to your tutor or other classmates’.
In contrast, some students found MASK-EDTM simulation less safe and even intimidating. Some students felt disconcerted in the initial simulation session by not knowing who was wearing the mask. Later, when students were aware that the mask was being worn by one of the lecturers, some students reported feeling intimidated by the potential for such detailed judgement of their performance:
‘If it was an actual old person, I would be more OK to talk to them, but because it was my teacher, and I knew she would be analysing everything I was saying, I was a bit more hesitant to say certain things’.
The group work setting was perceived by some students as a safety net, as they could ‘hide’ from engagement with the character if they were observing the situation rather than physically performing skills in the scenario. This group setting may jeopardise the authenticity of the learning experience for some, particularly with more introverted or less confident students:
‘In a group situation you can hide very easily … But in the real world it’s just you and this person’.
‘I remember when we did the first session everyone was going “no I’m not doing it, I just want to watch” … I guess if you force people to do it, you say groups of two, … everyone’s going to have the talk’.
‘Because that’s the thing, when you’re on placement it’s not as if you’re in a group of four and you can hide behind anyone else’.
Further to this, students would have liked more expert guidance from a second tutor in preparing to interact with the MASK-EDTM character. A majority of students mentioned that group feedback after the simulation session was inadequate because it was not sufficiently personalised:
‘I thought there would have been a lot better if each individual group had a separate time allocated to receive their feedback rather than just having it as like a sort of general one’.
There were several aspects of the importance of communication that students reported. Many described how MASK-EDTM simulation helped them refine the clarity and simplicity of their interpersonal communication, both in extracting information from their patients and providing instructions to them:
‘Even the instructions were like “you’ve got to take five steps forwards”, instead of saying … a huge sentence … [this] is something that I had to learn to … make an adjustment to’.
‘About jargon especially with explaining treatment techniques … simplified as much as possible … although … you didn’t really understand it at the time, you are … learning those skills’.
‘Just explaining things in simple terms … A lot of people found it took like a couple of weeks to get good at just doing it really simple’.
Two students further raised that the character’s background (i.e., a retired physiotherapist) was a potential barrier for students to reduce jargon in their communication with her as they presumed she understood the various terms. They pointed out that most patients would not have that background and, therefore, simpler communication might be required:
‘I think it has its advantages in terms of her being able to communicate to us what we need to know and when we need to know it. But in terms of the real world, it’s not helpful’.
‘Even in terms of wording, jargon, that kind of thing … as a physio she gets that, but if she’s not a physio, which you know 99% of the populations aren’t, they’re not going to understand half the things you’re saying’.
Students also highlighted the non-linearity of patient communication as an authentic aspect of learning to communicate with the MASK-EDTM character, particularly for their subsequent experiences on clinical placement:
‘Whereas a real patient might go off on one tangent or you ask them one question and they tell you everything, and you have to pick out little bits for your subjective and it doesn’t flow like how you want it to’.
‘The benefit of Joyce to me was that she talked so much, and you had to interrupt her’.
‘I felt semi-prepared, but we could have done more on it … People not being able to shut up … it’s just such a real thing and there are so many times where getting better at interrupting is what we need to work on because it’s tough’.
Students also reported the value of learning how to negotiate with the MASK-EDTM character regarding treatment goals:
‘Not like she’s angry or aggressive, but doesn’t want to do something in particular, and you have to like negotiate a different sort of treatment’.
Some students also linked the challenges of this negotiation with their real-world clinical experiences and perceived the MASK-EDTM character could be even more resistant to better reflect patient reluctance in the real world:
‘I would have preferred Joyce perhaps to give you a bit more resistance and you have to kind of talk around why she needs to get out of bed, why she needs to do this and convince her into it … it’s just … not how I found it on placement. You often have to do a lot more talking around why we need to do this … and convince them into it’.
Many students mentioned a feature of MASK-EDTM simulation was the opportunity to practise communicating with an older person, which was inherently different from the communication style they would use with their peers:
‘[MASK-EDTM helped in] getting your language jargon-free, and general skills of talking to people and talking to an older generation’.
‘It was also good having exposure because we saw a lot of older patients, and I talk very casually and I caught myself out a lot of times on placement … sometimes they didn’t really like the way I talk, because I’m just so casual. So think it helps … Probably in speaking a little bit more nicely … [laughs]’.
Students further highlighted that MASK-EDTM simulation could be used to learn more diversity in communication skills, beyond that which they had encountered in their experiences in the classroom:
‘Going out on placement, all my patients had non-motor impairments. You went from being able to speak and get informed consent from people, to people with unreliable yes/no [responses], people who couldn’t communicate, or communicated in a different language without realising it’.
‘I think bringing Joyce in [for learning about health literacy would be helpful] because I didn’t realise how poor people’s health literacy is’.
Finally, students highlighted opportunities for scaffolding more communication skill development as part of the MASK-EDTM experience, for example, requiring them to practise documentation after an interaction, using appropriate terminology and abbreviations:
‘I think a bit more exposure to the terminology as well, because I don’t know if it was just me, but I found that I didn’t really realise that we had to document that kind of stuff when we went on placement’.
‘Yeah, and learning the abbreviations a lot more, because my notes by the end [of placement] were a lot more abbreviated than they were at the start’.
Two perspectives on performativity emerged from the student responses: 1) the ‘teacher in role’ and 2) students’ emerging professional identities. However, students also asserted that there were some limitations in terms of their professional development stage at which the MASK-EDTM performativity was most useful.
The participating students expressed a range of perceptions of the masked teacher in the role of a patient, in response to what McAllister, Searl et al. (2013, p. 1456) call the ‘power of the personal artistry and … the multi-faceted aspects of the role, and the planned but improvised nature of the encounters’.
For example, the MASK-EDTM simulation was frequently described by students in terms of the authenticity of the teacher-in-role performance and how the mask itself allowed students to suspend disbelief and engage with the character:
‘I thought it was just like having a different visual there, means you separated the two. Like she was a proper character instead of being [the lecturer]’.
‘Everyone was laughing, and I was like “Why are they laughing at this poor [person]?” ’
‘I didn’t know if it was [the lecturer] or not, it took me like 10 minutes’.
In contrast, some students found the mask somewhat distracting as they tried to guess who was behind it:
‘A disadvantage for a lot of people was the initial shock of trying to figure out what was behind the mask. That was really distracting. So a lot of people missed out on a lot of vital information at the start’.
This perspective was concerned with performativity in terms of the participating students’ construction and performance of their professional identities. It resonates with Doran and Setchell’s (2018, p. 127) assertion that ‘what constitutes a physiotherapist is not pre-existing: through repetition of particular bodily gestures, attitudes and acts of speech, the recognisable identity of a “physiotherapist” is formed’.
For instance, participating students described the MASK-EDTM encounter in terms of their need to perform physically in the role, demonstrating spontaneity and adaptability within the task’s physical aspects:
‘Like with students it’s fine because you’re seeing them all day but going in with [the MASK-EDTM character] you’re like … I don’t know if I could touch just there to help you sit up. So that was good to practise’.
‘You kind of have to think on your feet, so it worked on those skills’.
‘There are differences in potential of what I would have wanted to do with Joyce versus what she actually wanted out of me’.
‘[The lecturer] would act a lot frailer or sort of surprise you and keep you on your toes which is real life, and I felt like that was a good simulation to prepare’.
‘At the time I didn’t realise how beneficial it would have been to actually jump in and do it’.
Many students raised their appreciation of needing to step into the physiotherapist role and develop confidence using their ‘physio voice’ as an additional feature to engage with the simulated character. This included mindfulness of the patient’s psychological and cultural safety, for example, preserving their modesty when mobilising them out of bed after surgery. Often the first step in this interaction was establishing rapport and ensuring they interacted with the character in an appropriately respectful way:
‘Just sort of like that rapport and that interaction, just between the two of you’.
‘Cause we were in class and we just take our shirts off and run over. But I remember going to get Joyce out of bed and we had to put the gown over and everything … and like we’d have ladies who were like, “Oh I’m wearing my singlet, I don’t want to wear just my singlet”’.
Students also described other ways that the MASK-EDTM simulation tested their skills and knowledge during their performance in a formative way:
‘So it kind of made us test what we already knew, and I thought that was really helpful to see what stage you were at and that you were actually able to conduct a subjective [assessment] on just what you knew’.
However, while students recognised the value of testing their manual handling skills, several articulated that more practice, and with different types of characters, would be valuable to prepare them for clinical placement:
‘We did mobilising of Joyce so we got to practise those skills and looking for attachments’.
‘I think one thing we could have done a bit more is the manual handling side of things … [on clinical placement] we had a lot of obese patients that were like three max assist to sit out of bed … so being able to work as a team … if you’re the one coordinating, who should go where and what to do. We were all a bit timid at the start but once you get into placement you realise you need to get like right on top of them basically’.
While the performative nature of the MASK-EDTM simulation was seen to bring many advantages, there was also a clear consensus from the students that the simulation was not superior to practising skills with real patients:
‘I believe the real patients in neuro classes were more helpful than MASK-EDTM’.
‘However [I] learnt the majority of how to cope within first two weeks of placement’.
‘When you’re in hospital and you’re having to do it all the time it kind of sticks more’.
More specifically, students indicated that the value of MASK-EDTM simulation is greater prior to authentic clinical exposure:
‘Now that I’ve seen real patients, I don’t think that MASK-EDTM would be that helpful’.
‘I think earlier [in the curriculum] is better, once you get back from placement, I think you have more of an understanding about how the patients actually are’.
This study suggests that, on the whole, physiotherapy students perceive MASK-EDTM simulation as highly valuable for enhancing classroom learning and in preparing for clinical placement before attending their first clinical placement. In particular, students felt that MASK-EDTM simulation improved their ability to apply theory to practice, engage with material covered in the unit, remember practical aspects of the lesson, prepare for practical exams, self-reflect and learn from mistakes in a safe environment, receive effective feedback and engage with peer learning. They also reported an increase in confidence in engaging with an older person; developing rapport, empathy and communication skills; implementing manual handling skills; managing attachments; and their sense of preparedness for their physiotherapist role in a clinical setting. This enhanced self-reported readiness for practice in the real world is consistent with evidence from studies of MASK-EDTM in nursing students (Kable et al. 2013).
However, physiotherapy students felt the usefulness of MASK-EDTM diminished somewhat after completing a clinical placement. It is perhaps not surprising that students perceived the utility of classroom-based simulation to be lower after real-world clinical learning due to several inherent limitations of simulation that become evident after real-world clinical exposure. Firstly, while MASK-EDTM allows students to interact with an authentic patient in an authentic physical environment, it is not in an authentic context. For example, there were no other health professionals, patients, volunteers, or visitors present for the MASK-EDTM simulation in our model. Secondly, in contrast to ongoing episodes of care, the MASK-EDTM simulation occurred as isolated episodes of care. As such, MASK-EDTM simulation did not provide the same experience of continuity of care that clinical placements provide. Thirdly, while MASK-EDTM is relevant and authentic, it is still a form of simulation. Even the most sophisticated simulation experience is unlikely to fully replicate the multifactorial immersive experience of the authentic clinical environment. Students’ perception that MASK-EDTM is less useful after clinical placement suggests that care should be taken in selecting the timing of MASK-EDTM within the course of student learning. Giving students exposure to MASK-EDTM prior to any clinical placements is likely to be most useful and may increase students’ confidence when commencing clinical placements. It suggests that students valued clinical placements more highly for learning clinical skills. Therefore, MASK-EDTM simulation, as applied in this study, should only be used as an adjunct and not an alternative to clinical placement. Thus, the value of MASK-EDTM in the current sequence appears to be that of students’ developmental preparation prior to placement. Once they have reached the necessary level of preparedness to go on placement, the real-life experience of clinical contact with patients is likely to supersede the simulated patient experience.
The importance of authenticity was evident across the key themes identified in the analysis of focus group discussions. While creating a safe learning environment was clearly a pillar of MASK-EDTM simulation’s success, the perceived authenticity of the activity had different meaning for different students in terms of psychological safety. There were varying degrees to which students could suspend their knowledge about the educator’s identity under the mask; this affected their willingness to engage and take risks within the learning activity. Nonetheless, most students recognised the value of practising both practical and communication skills in a setting that more closely mirrored that which they would encounter on clinical placement. We know that adult learners are motivated to learn when the learning activity is perceived to be relevant and has real-world application (Knowles 1984). In this way, MASK-EDTM meets the requirements of being a motivating learning strategy.
The performative aspect of MASK-EDTM simulation afforded spontaneous learning moments, which students valued as more authentic than practising with peers. The students described developing confidence in stepping into the physio role that extended beyond simple technical proficiencies to an appreciation of how to approach the character as a person deserving of dignity and respect (e.g., ensuring the preservation of patient dignity). Through interacting with the MASK-EDTM character, students could refine their ‘physio voice’ in a safe learning environment in tandem with developing communication and technical skills. Overall, the performative aspects of the MASK-EDTM simulation, while unscripted and unique for each student, may provide rich opportunities for developing a physiotherapist professional identity—treating not just pathology but also people.
Some students’ suggestions to improve the authenticity and value of MASK-EDTM are insightful (e.g., increasing character complexity and incorporating a broader range of communication limitations), while some are challenging to implement (e.g., a ratio of two students for each character encounter). A crucial feature of MASK-EDTM character development is ensuring it is student friendly and that the student never feels rebuked or shamed by the character in any way, such that the student can develop confidence throughout the simulation (Reid-Searl et al. 2011). Adding more challenging patient attributes (such as limited verbal communication) might only be appropriate once students have established confidence in the MASK-EDTM process. The higher ratio of character to students (i.e., interacting in pairs rather than groups) could be unfeasible due to the educator’s fatigue inside the mask, particularly for larger cohorts. Thus, the scalability of MASK-EDTM remains a limiting factor for future simulation design based on these insights.
Students acknowledged that the presence of an academic behind the mask during MASK-EDTM simulation allows for accurate and timely feedback. For many, this also enhanced the perceived safety of the learning environment. The presence of an expert is also supported by Vygotsky’s (1978) sociocultural theory of education, particularly, his concept of the zone of proximal development that he defined as ‘the distance between the actual developmental level [of the learner] as determined by independent problem solving, and the level of potential development as determined through problem solving under guidance … or in collaboration with more capable peers’ (p. 86). The suggestion that having a second tutor present would enhance the quality of feedback has merit, although resource limitations in the university context may hamper implementation.
This study explored students’ perceptions of the value of MASK-EDTM, including perceived readiness for clinical placement. Still, future research should examine whether MASK-EDTM exposure affects clinical performance as measured by a standardised clinical assessment tool. A robust test of the efficacy of MASK-EDTM would be valuable to physiotherapy educators around the world who strive to optimise curriculum design to best prepare their students for real-world experience.
Physiotherapy students perceive MASK-EDTM simulation as valuable in enhancing classroom-based learning relating to clinical practice across various skills, including manual handling, developing rapport and empathy, and communicating and engaging with an older person. Prior to clinical placement, MASK-EDTM helps develop a student’s ability to step into the physiotherapist role through honing the performance of both technical and communication skills in a safe learning environment. Future studies should explore the utility of MASK-EDTM in other clinical areas of physiotherapy and its effect on clinical performance in the real world.
We would like to thank Professor Kerry Reid-Searl for her guidance, as well as all the students who volunteered their time to participate in this study.
Barsuk, JH, McGaghie, WC, Cohen, ER, O’Leary, KJ & Wayne, DB 2009, ‘Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit’, Critical Care Medicine, vol. 37, no. 10, pp. 2697–2701.
Braun, V & Clarke, V 2008, ‘Using thematic analysis in psychology’, Qualitative Research in Psychology,vol. 3, no. 2, pp. 77–101.
Cooper, S & Endacott, R 2007, ‘Generic qualitative research: a design for qualitative research in emergency care?’, Emergency Medicine Journal, vol. 24, no. 12, pp. 816–819.
Creswell, J 2009, ‘Editorial: mapping the field of mixed methods research’, Journal of Mixed Methods Research, vol. 3, pp. 95–108.
Doran, B & Setchell, K 2018, ‘Performative acts of physiotherapy’, Manipulating practices. A critical physiotherapy reader, Capellen Damm Akademisk, Oslo, Norway.
Fraser, K, Peets, A, Walker, I, Tworek, J, Paget, M, Wright, B & McLaughlin, K 2009, ‘The effect of simulator training on clinical skills acquisition, retention and transfer’, Medical Education, vol. 43, no. 8, pp. 784–789.
Jeffries, PR 2005, ‘A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing’, Nursing Education Perspectives, vol. 26, no. 2, pp. 96–103.
Kable, AK, Arthur, C, Levett-Jones, T & Reid-Searl, K 2013, ‘Student evaluation of simulation in undergraduate nursing programs in Australia using quality indicators’, Nursing & Health Sciences, vol. 15, no. 2, pp. 235–243.
Knowles, M 1984, The adult learner: a neglected species, Gulf Publishing, Houston, TX.
McAllister, M, Levett-Jones, T, Downer, T, Harrison, P, Harvey, T, Reid-Searl, K, Lynch, K, Arthur, C, Layh, J & Calleja, P 2013 ‘Snapshots of simulation: creative strategies used by Australian educators to enhance simulation learning experiences for nursing students’, Nurse Education in Practice, vol. 13, no. 6, pp. 567–572.
McAllister, M, Searl, KR & Davis, S 2013, ‘Who is that masked educator? Deconstructing the teaching and learning processes of an innovative humanistic simulation technique’, Nurse Education Today, vol. 33, no. 12, pp. 1453–1458.
Reid-Searl, K, Eaton, A, Vieth, L & Happell, B 2011, ‘The educator inside the patient: “students” insights into the use of high fidelity silicone patient simulation’, Journal of Clinical Nursing, vol. 20, no. 19–20, pp. 2752–2760.
Reid-Searl, K, Happell, B, Vieth, L & Eaton, A 2012, ‘High fidelity patient silicone simulation: a qualitative evaluation of nursing “students” experiences’, Collegian, vol. 19, no. 2, pp. 77–83.
Sturm, LP, Windsor, JA, Cosman, PH, Cregan, P, Hewett, PJ & Maddern, GJ 2008 ‘A systematic review of skills transfer after surgical simulation training’, Annals of Surgery, vol. 248, no. 2, pp. 166–179.
Vygotsky LS 1978, Mind in society, Harvard University Pres