Primary care pharmacists’ knowledge and their perception of primary
healthcare professionals’ role in managing inflammatory bowel disease: a
cross-sectional study in Australia
Sharmila S Prasad 1, 2 *, Simon Keely 1, 2, Nicholas J Talley 2, 3, Kerith Duncanson 2, 4,
Therése Kairuz 1, Michael P Jones 5, Marjorie M Walker 2, 3.
Abstract
Purpose:
Inflammatory bowel disease (IBD) management is complex and challenging,
requiring a multidisciplinary approach. While pharmacists may play a
key role as the first point of contact for patients with initial
symptoms or disease relapse, there is scant literature on pharmacists’
knowledge in IBD management. We conducted a survey exploring
pharmacists’ knowledge, potential educational needs and their
perception of pharmacists and other healthcare professionals’ roles in
managing patients with IBD.
Design and Methodology:
An online survey was distributed to pharmacists through professional
organisations. The survey included questions about demographic
information, concepts related to IBD management, and the roles of
pharmacists and healthcare professionals in managing patients with IBD.
Findings:
Fifty-two respondents completed the survey (response rate could not be
determined). The overall knowledge score for the majority of
respondents was categorised as ‘low’ to ‘average’. Pharmacists
demonstrated the highest level of accuracy in their knowledge scores
regarding their understanding of the role and importance of vaccination
in IBD (94.2%; n = 49). Pharmacists who had exposure to patients with
IBD demonstrated better knowledge scores than those without exposure to
IBD patients in their practice (p = 0.005). Further, general
practitioners (GPs) were perceived as the key care providers to IBD
patients, while pharmacists considered themselves as equally important
in providing medication-related information to patients.
Conclusion:
This study indicated that pharmacists’ knowledge of IBD and its
management was suboptimal; however, with education and training, there
are opportunities for pharmacists to play a more active role in
managing patients with IBD.
Keywords: inflammatory bowel disease (IBD), pharmacist, healthcare
professionals, knowledge, perception
1
School of Biomedical Science and Pharmacy, Faculty of Health and
Medicine, University of Newcastle, Callaghan, New South Wales 2308,
Australia.
2
NHMRC Centre of Research Excellence in Digestive Health, University of
Newcastle, New Lambton Heights, New South Wales 2305, Australia.
3
School of Medicine and Public Health, Faculty of Health and Medicine,
University of Newcastle, New Lambton Heights, New South Wales 2305,
Australia.
4
School of Health Science, Faculty of Health and Medicine, University of
Newcastle, New Lambton Heights, New South Wales, New South Wales 2305
Australia.
5
Psychology Department, Macquarie University, Macquarie Park, Sydney, New
South Wales 2109, Australia.
Corresponding author:
Sharmila S Prasad, School of Biomedical Science and Pharmacy, Faculty of
Health and Medicine, University of Newcastle, University Dr NSW 2308,
Australia, [email protected]
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic disease affecting the
gastrointestinal tract. It usually presents as one of two common forms:
ulcerative colitis and Crohn’s disease (Gastroenterological Society of
Australia 2018; Karimi et al. 2020). Symptoms include chronic abdominal
pain, diarrhoea, anaemia, loss of appetite, fatigue, weight loss and
extraintestinal complications. IBD is also characterised by cycles of
remission and relapse (Gastroenterological Society of Australia 2018;
PricewaterhouseCoopers Australia 2013). There is a poor quality of life
with a mental health burden affecting patients’ personal, social and
professional life (Mikocka-Walus et al. 2020). Inflammatory bowel disease
is most common among those aged between 15 and 40 years. Although mortality
rates are considered low, IBD is incurable and lifelong, further
contributing to the economic burden of the disease (Gastroenterological
Society of Australia 2018; Karimi et al. 2020).
In developed nations, IBD has a disproportionately high economic burden.
For example, in Australia, IBD is responsible for an estimated annual cost
of approximately AU$2.7 billion, with hospital costs nationally in excess
of AU$100 million (Deloitte Access Economics Pty Limited 2007;
PricewaterhouseCoopers Australia 2013). Optimal management of patients with
IBD requires prevention of disease relapse, maintenance of remission and
avoidance of adverse effects along with better quality of life (Georgy,
Negm & El-Matary 2019; Massuger et al. 2019). Medication management is
the keystone for treating patients with IBD (Gastroenterological Society of
Australia 2018; Georgy, Negm & El-Matary 2019). The treatment of IBD
has advanced in recent years, making medical therapy more effective;
however, it has also become more complex with the use of corticosteroids,
immunosuppressants and biological therapies that have risk-benefit profiles
that require careful monitoring (Blackburn et al. 2019; Zezos & Panisko
2018).
In a recent systematic review, the authors highlighted the potential
opportunities in the management of IBD through proven pharmacist
interventions in other chronic diseases, leading to improved patient
outcomes, including quality of life, disease management and self-management
(Prasad, Duncanson et al. 2020). Understanding such factors will likely
lead to better IBD management that maximises therapeutic efficacy and
minimises the potential for adverse effects (Massuger et al. 2019).
Pharmacists often act as intermediaries between doctors and patients by
providing easily accessible clinical advice and medicines without needing a
pre-booked appointment (International Pharmaceutical Federation 2019;
Manolakis & Skelton 2010). They are generally the initial source of
contact for patients with minor gastrointestinal ailments because of the
over-the-counter (OTC) medications that can play a critical role in their
care (Blackburn et al. 2019). Therefore, engagement of pharmacists provides
an opportunity for improving clinical outcomes in a primary care setting
(Blackburn et al. 2019; Manolakis & Skelton 2010).
Factors such as gender, pharmacist’s age group and familiarity with IBD
patients are important in understanding the association on knowledge and
perception among healthcare professionals (Carvajal et al. 2013; Janzen et
al. 2013). While there is published literature available on knowledge,
attitudes and perceptions of healthcare professionals with regards to IBD,
the focus is mainly on secondary or tertiary care with a small proportion
addressing primary care relating to general practitioners (GPs) (Bennett,
Munkholm & Andrews 2015; Crohn’s & Colitis Australia 2017;
Mikocka-Walus et al. 2014; Tan et al. 2012). No published literature has
assessed pharmacists’ knowledge and perception of IBD management. A recent
study evaluated pharmacists’ confidence levels in the care and management
of IBD and reported that pharmacists lacked sufficient confidence in
managing IBD (Prasad, Keely et al. 2020). To address this gap, this study’s
primary aim was to ascertain pharmacists’ existing knowledge and
educational needs for managing IBD in the primary care setting. A second
aim was to explore factors influencing perception(s) of pharmacists as
healthcare professionals managing patients with IBD.
METHODS
STUDY PARTICIPANTS
Inclusion criteria for the study were: 1) pharmacists who had completed
either a Bachelor or a Master of Pharmacy, 2) registered with the Australia
Health Practitioner Regulation Agency (Ahpra), 3) were working in a primary
care setting (i.e., a community pharmacy/general practice/clinic and/or
accredited to conduct medication reviews) (The Department of Health 2013).
Registered pharmacists work in various practice settings and must complete
a minimum of 150 hours per year working within a primary or secondary care
setting to maintain their registration as a practising pharmacist
(Pharmaceutical Society of Australia 2019; Pharmacy Board of Australia
AHPRA 2020). The survey was open from August 2019 to April 2020 (terminated
due to COVID-19), during which there were approximately 31,503 pharmacists
registered in Australia (Pharmacy Board of Australia AHPRA 2020). The data
on the number of registered pharmacists working in a primary care setting
was not available at the time of the study. Therefore, the sample size
required was calculated using a confidence interval for a single
proportion, factoring in an anticipated response rate of 15–30% (Charan
& Biswas 2013; Phillips et al. 2017). The minimum required sample size
was estimated at 49–80 pharmacists with a confidence level of 95% and a 5%
margin of error. A response rate could not be calculated due to the lack of
available data to determine the exact number of registered pharmacists
working in a primary care setting at the time of the study.
Convenience sampling of pharmacists in the Hunter region was the primary
recruitment strategy. This was supplemented by snowballing, where
participants (pharmacists) who were already enrolled helped promote the
study by informing friends and colleagues about the research and directing
interested individuals to the researchers. In addition, pharmacists were
recruited indirectly through professional organisations (i.e., the
Pharmaceutical Society of Australia, Newcastle, the Hunter Valley
Pharmacists Association, the Pharmacy Guild of Australia and the Australian
Association of Consultant Pharmacy across the broader profession within
Australia). The survey could only be accessed and completed via the link
provided in the participant invitation information. Completion of the
survey by pharmacists were deemed as consent for the study, specified in
the participant information sheet included at the start of the survey.
STUDY DESIGN
This exploratory cross-sectional survey study used a questionnaire that was
developed from a review of the literature and of systematic reviews
relating to pharmacists’ role in chronic disease and the management of IBD
(Prasad, Duncanson et al. 2020; Prasad, Keely et al. 2020; Prasad, Potter
et al. 2020). The questionnaire was piloted for content and faced validity
among a sample of 10 healthcare professionals (two gastroenterologists, six
pharmacists, one GP and a research physician in the field of IBD). Based on
the results of the pilot, the final questionnaire was uploaded to Research
Electronic Data Capture (REDCap), a secure web application designed for
clinical and translational survey research.
The questionnaire was anonymous, self-administered, delivered
electronically and consisted of three domains that took approximately 20
minutes to complete. It included demographic information (e.g., age,
gender, previous practice, current practice including a secondary role,
qualifications), questions seeking to elicit pharmacists’ level of
knowledge (20 questions about general concepts related to IBD and specific
concepts of IBD management) and perceptions regarding the management of IBD
(pharmacists’ perception of themselves and of other healthcare
professionals).
Pharmacists were assessed for their knowledge about concepts of IBD that
ranged from general concepts (i.e., prevalence, age of diagnosis, causes of
IBD, inflammation associated with IBD, symptoms and food triggers) to more
advanced IBD management concepts (i.e., complications associated with IBD,
impact of smoking in IBD, medication usage in IBD that related to
contradiction, opioid use, pregnancy, biologics, immunosuppressive agents
and types of vaccination in IBD). Individual scores for the participants’
level of knowledge were expressed as an average percentage of the maximum
possible score (100%). The overall knowledge score was categorised as: 0%
deemed not knowledgeable, <25% very low knowledge, 25–50% low knowledge,
51–75% average knowledge and >75% adequate knowledge.
To determine pharmacists’ perceived level of confidence relating to IBD,
respondents were asked to complete a pre- and post-self-evaluation of five
components related to IBD management included in the knowledge domain of
the questionnaire. This self-evaluation is based on experiential learning,
a holistic educational philosophy by David Kobased on the individual’s
experiences influencing their education, learning and understanding of new
knowledge (Chamane, Kuupiel & Mashamba-Thompson 2019). Questions were
largely formatted as binary (yes/no), multiple choice, 5-point Likert scale
responses, ranking and open-ended text. The questionnaire is available on
request from the authors. A current practice setting was recorded to
differentiate between the principal role (where the pharmacist spent most
of their working week) and the secondary role, as some pharmacists are
employed at more than one site or in more than one sector. For rigour,
strengthening the reporting of observational studies in epidemiology
(STROBE) statement was used (von Elm et al. 2007).
STATISTICAL ANALYSIS
Descriptive data were analysed using median with an interquartile range and
frequency (%) to describe the demographics of the participants and
knowledge concepts in IBD. Free text responses were categorised into
correct or incorrect responses to be included in the analysis. Descriptive
statistics and non-parametric tests (Mann Whitney U Test/Wilcoxon Rank Sum
Test and Kruskal-Wallis) were used to explore difference in scores of
pharmacists’ perception of their role managing IBD before and after
completing the knowledge section. The overall knowledge scores were
analysed using frequencies (%). Possible relationships between pharmacists’
knowledge of IBD and demographic characteristics were evaluated with
Mann-Whitney-Wilcoxon test for two groups and Kruskal-Wallis test for more
than two groups. Statistically significant differences were declared at a
p-value of less than 0.05. Analysis of the data was performed using Stata
version 14 statistical software (StataCorp. Stata Statistical Software:
Release 14. College Station, TX: StataCorp LP. 2015).
RESULTS
PARTICIPATION INFORMATION
A total of 52 responses were received between August 2019 and April 2020.
The demographic information of respondents is shown in Table 1. The
majority of respondents were aged 25–44 years (65.4%, n = 34), and more
than half were female (n = 32, 61.5%). Approximately 71% of respondents had
completed a Bachelor’s qualification, and 32.7% (n = 17) had additional
postgraduate qualifications. Regarding the years of experience, having more
than 10 years of experience was most common (n = 23, 44%). Hours of work
had a similar distribution in all three groups.
Table 1: Background characteristics of the study participants (n=52)
|
Variables
|
Frequency (n)
|
Percent (%)
|
|
Age groups (years)
|
|
18–24
|
6
|
11.5
|
|
25–34
|
17
|
32.7
|
|
35–44
|
17
|
32.7
|
|
45+
|
12
|
23.1
|
|
Gender
|
|
Male
|
20
|
38.5
|
|
Female
|
32
|
61.5
|
|
Qualification
|
|
Bachelor of Pharmacy
|
37
|
71.1
|
|
Master of Pharmacy
|
15
|
28.9
|
|
Attended postgraduate
|
|
Yes
|
17
|
32.7
|
|
No
|
35
|
67.3
|
|
Length of experience (years)
|
|
≤5
|
15
|
28.9
|
|
6–10
|
14
|
26.9
|
|
10+
|
23
|
44.2
|
|
Length of working hours per week (hours)
|
|
≤29
|
18
|
34.6
|
|
30–39
|
17
|
32.7
|
|
40+
|
17
|
32.7
|
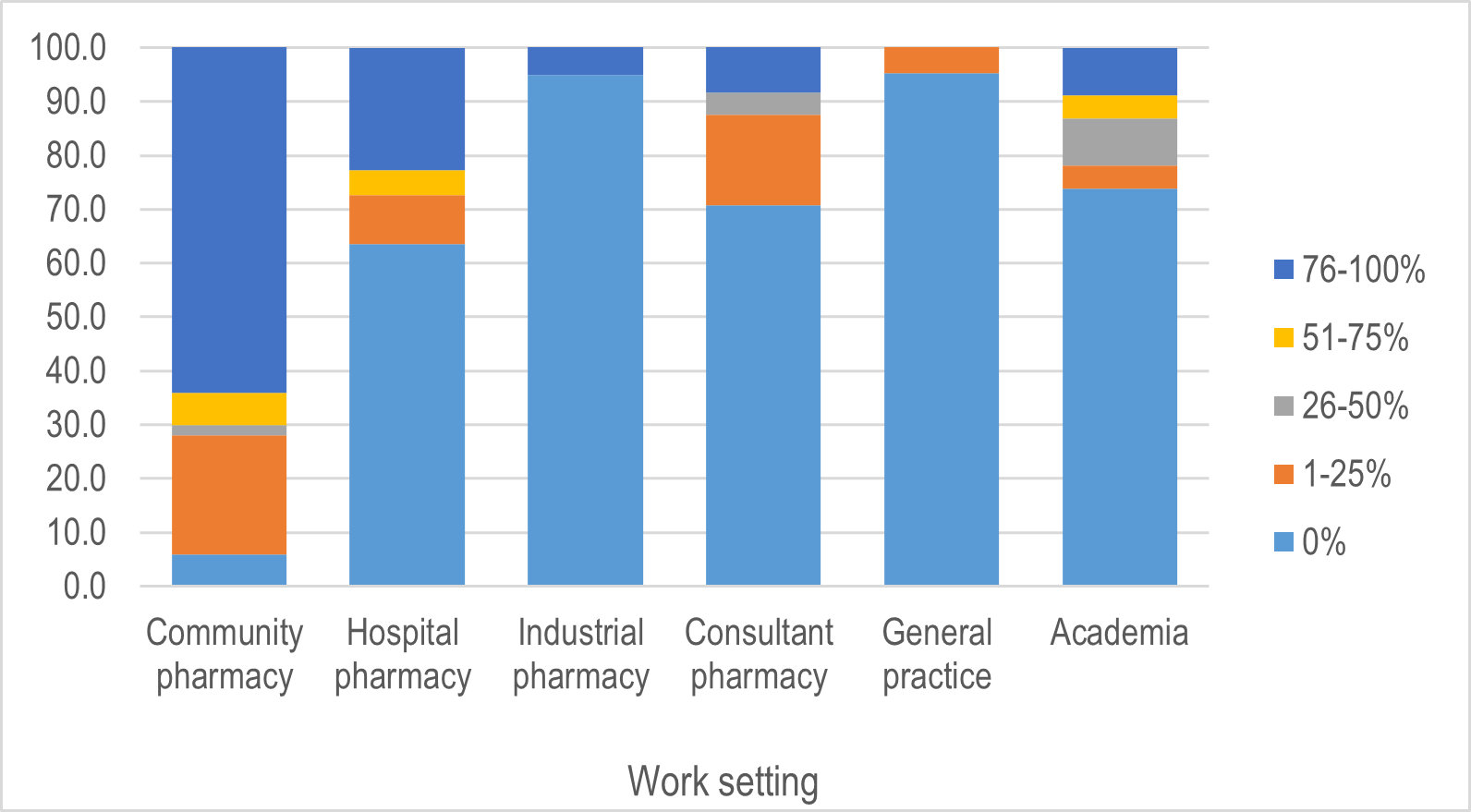
There was a variety of reported practice settings. In their principal role,
64% (n = 32) of respondents were employed in a community pharmacy setting,
22.7% (n = 5) in a hospital pharmacy setting, 8.7% (n = 2) in academia,
8.3% (n = 2) as consultant pharmacists, 5% (n = 1) in industry pharmacy and
0% (n = 0) in a general practice setting (Figure 1). As a secondary role,
30% (n = 15) worked in a community pharmacy setting, 20.9% (n = 5) as
consultant pharmacists, 17.3% (n = 4) in academia, 13.5% (n = 3) in a
hospital pharmacy setting, 4.8% (n = 1) in a general practice setting and
0% (n = 0) in industry pharmacy.
Figure 1. Proportion of time spent in various workplace settings of
pharmacists who completed the survey on inflammatory bowel disease (IBD)
perceptions and knowledge.
PHARMACISTS' LEVEL OF IBD KNOWLEDGE
Variables such as age, gender, educational levels, length of experience and
exposure to patients with IBD were analysed to determine their association
with pharmacists’ knowledge. Pharmacists had low (median score range:
26–50) to average (median score range: 51–75) levels of knowledge (Table
2). A statistically significant difference in the overall knowledge score
was observed based on the pharmacists’ exposure to patients with IBD (p =
0.005) in their practice, with no other statistically significant
associations identified (Table 2).
Table 2. The association between background characteristics and
pharmacists’ knowledge of IBD (n=52)
|
Variables
|
Overall knowledge score*
Median (IQR)
|
P-value
|
|
Age group (years)**
|
|
18–24
|
50.6 (38.1, 52.4)
|
0.05
|
|
25–34
|
63.1 (58.3, 72.6)
|
|
|
35–44
|
70.2 (53.6, 78.6)
|
|
|
45+
|
63.1 (51.2, 75.6)
|
|
|
Gender***
|
|
Male
|
58.3 (49.4, 73.2)
|
0.37
|
|
Female
|
63 (53.6, 77.4)
|
|
|
Qualification***
|
|
Bachelor of Pharmacy
|
63.1 (42.8, 77.3)
|
0.86
|
|
Master of Pharmacy
|
63.1 (52.4, 72.6)
|
|
|
Attended postgraduate***
|
|
Yes
|
67.8 (54.7, 73.8)
|
0.31
|
|
No
|
59.5 (48.8, 78.6)
|
|
|
Length of experience (years)**
|
|
≤5
|
59.5 (47.6, 72.6)
|
0.48
|
|
6–10
|
63.1 (57.1, 78.6)
|
|
|
11+
|
70.2 (53.6, 77.4)
|
|
|
Length of working hours per week (hours)**
|
|
≤29
|
64.9 (50.0, 82.1)
|
0.62
|
|
30–39
|
63.1 (54.8, 77.4)
|
|
|
40+
|
59.5 (52.4, 71.4)
|
|
|
Exposure to IBD patients***
|
|
Yes
|
64.3 (53.6, 77.4)
|
0.005
|
|
No
|
36.9 (25, 42.8)
|
|
*
Medians with an interquartile range were used to present the overall
knowledge score by pharmacists’ characteristics. Comparison between
categorical variables were made by using the Kruskal-Wallis Test (**)
or the Mann-Whitney-Wilcoxon Test (***); IBD = Inflammatory Bowel
Disease.
Pharmacists who had exposure to IBD patients in their practice scored
higher for IBD knowledge (overall score median 64.3) than those without any exposure or experience with IBD patients (overall score median 36.9). There was a statistically significant trend associated with knowledge and the pharmacists’ age (p = 0.05). Those aged 35–44 years had higher overall
scores for knowledge of IBD compared to other age groups (18–24 years,
25–34 years and 45+ years).
Of the 20 knowledge questions, 11 questions (55%) were answered correctly,
and one question reported equal responses (n = 26; 50%) of correct and
incorrect by the respondents (Table 3).
Table 3. Participants’ responses to the knowledge questions of the survey (n=52)
|
Topic concepts in IBD
|
Correct (percentage)
|
|
Cause(s) of IBD*
|
48 (92.3%)
|
|
Source of inflammation in IBD
|
43 (82.7%)
|
|
Possibility of a cure in IBD
|
38 (73.1%)
|
|
GI complications
|
38 (73.1%)
|
|
Associated risk of smoking in IBD
|
18 (34.6%)
|
|
Food triggers associated with IBD
|
47 (90.4%)
|
|
IBD prevalence
|
18 (34.6%)
|
|
Age of diagnosis in IBD
|
48 (92.3%)
|
|
IBD symptoms
|
47 (90.4%)
|
|
Issues related to extraintestinal complications
|
18 (34.6%)
|
|
OTC medication use related to toxic megacolon
|
19 (36.5%)
|
|
Use of immunosuppressive medications
|
39 (75.0%)
|
|
Contraindicated medications in IBD
|
21 (40.4%)
|
|
Importance of iron supplementation
|
26 (50.0%)
|
|
Drugs in pregnancy**
|
44 (84.6%)
|
|
Opioid use in IBD
|
43 (82.7%)
|
|
Role of biologics in therapy
|
20 (38.5%)
|
|
Colon cancer screening
|
8 (15.4%)
|
|
Vitamin deficiencies
|
23 (44.2%)
|
|
Importance of vaccinations in IBD
|
49 (94.2%)
|
Frequency (%) was used to present the level of knowledge of
pharmacists; responses were scored as correctly answered = 100% and
incorrectly answered = 0%. * Responses were categorised as: 4 correct =
100%, 3 correct = 75%, 2 correct = 50%, 1 correct = 25% and incorrect =
0%. ** Responses were categorised as: 8 correct answers = 100%, 5–7
correct = 75%, 4 correct = 50%, 1–3 correct = 25% and incorrect = 0%;
IBD = inflammatory bowel disease; GI = gastrointestinal; OTC =
over-the-counter.
The overall knowledge score for the respondents showed that one pharmacist
(1.9%) was categorised as has having very low knowledge (score 1–25%); 21
pharmacists (40.4%) were categorised equally as having low (score 26–50%)
and average knowledge (score 51–75%); and nine pharmacists (17.3%) were
deemed as having adequate knowledge (score >75%). Inflammatory bowel
disease concepts that showed the highest level of pharmacists’ knowledge
included importance of vaccinations in IBD (n = 49; 94.2% correct
responses), cause of IBD and age of diagnosis (n = 48; 92.3% correct
responses), food triggers and IBD symptoms (n = 47; 90.4% correct
responses), drugs in pregnancy (n = 44; 84.6% correct responses) and source of inflammation and opioid use (n = 43; 82.7% correct responses). Concepts where pharmacists had lower knowledge included colon cancer screenings (n = 8; 15.4% correct responses), risks associated with smoking, prevalence and extraintestinal complications in IBD (n = 18; 34.6% correct responses), OTC medicines associated with toxic megacolon (n = 19; 36.5% correct responses) and place in therapy for biologics (n = 20; 38.5% correct responses).
PHARMACISTS' IBD KNOWLEDGE: PERCEPTIONS AND SELF-REFLECTIONS
A pre- and post-evaluation of changes in perceptions and the related
association with demographics was undertaken. Overall, the median sum score for each of the five components showed that pharmacists perceived
themselves to be better in four out of the five components (understanding
IBD, providing information, providing additional support and addressing
patient needs) before taking the knowledge section of the questionnaire
when compared to the median sum score of their perception after the
knowledge section. As shown in Table 4, educational level (initial or
postgraduate qualifications), length of experience and length of working
hours per week were not significantly associated with any change in
pharmacists’ perception regarding their current knowledge. However, there
were statistically significant associations between change in pharmacists’
perception and age, gender and exposure to patients with IBD (all
p<0.05). Pharmacists aged 35–44 years, females and those who had
experience with IBD patients perceived themselves as having better
knowledge (higher mean scores) prior to completion of the knowledge section when compared to their scores (lower mean scores) after completing the knowledge section.
Table 4. The association between background characteristics and change in
pharmacists’ perception pre- and post-completion of knowledge section (n=52)
|
Variables
|
Overall perception pre-completion of the knowledge section*
|
Overall perception post-completion of the knowledge
section*
|
P-value
|
|
Age group (years)**
|
|
18–24
|
50 (50, 50)
|
50 (50, 75)
|
0.054
|
|
25–34<
|
50 (50, 75)
|
50 (50, 75)
|
|
|
35–44
|
75 (75, 75)
|
50 (50, 75)
|
|
|
45+
|
50 (50, 62.5)
|
50 (50, 75)
|
|
|
Gender***
|
|
Male
|
50 (50, 75)
|
62.5 (50, 75)
|
0.008
|
|
Female
|
75 (50, 75)
|
50 (50, 75)
|
|
|
Qualification***
|
|
Bachelor of Pharmacy
|
50 (50,75)
|
50 (50, 75)
|
0.84
|
|
Master of Pharmacy
|
75 (50,75)
|
50 (50, 75)
|
|
|
Attended postgraduate***
|
|
Yes
|
50 (50, 75)
|
50 (50, 50)
|
0.27
|
|
No
|
75 (50, 75)
|
50 (50, 75)
|
|
|
Length of experience (years)**
|
|
≤5
|
50 (50, 75)
|
50 (50, 75)
|
0.19
|
|
6–10
|
62.5 (50, 75)
|
50 (50, 75)
|
|
|
11+
|
75 (50, 75)
|
50 (50, 75)
|
|
|
Length of working hours per week (hours)**
|
|
≤29
|
75 (50, 75)
|
50 (50, 75)
|
0.09
|
|
30–39
|
50 (50, 75)
|
50 (50, 75)
|
|
|
40+
|
50 (50, 75)
|
50 (50, 75)
|
|
|
Exposure to IBD patients***
|
|
Yes
|
75 (50, 75)
|
50 (50, 75)
|
0.044
|
|
No
|
25 (0, 50)
|
50 (25, 50)
|
|
*
Medians with an interquartile range were used to present the overall
knowledge score by pharmacists’ characteristics. Comparisons between
categorical variables were made using Kruskal-Wallis Test (**) or
Mann-Whitney-Wilcoxon Test (***); IBD = inflammatory bowel disease.
PHARMACISTS' PERCEPTIONS ON THE ROLE OF HEALTHCARE PROFESSIONALS MANAGING IBD
The section of the questionnaire that related to pharmacists’ perceptions
on the roles of healthcare professionals in primary care assessed which
healthcare professional they thought patients would consult on key aspects
of managing IBD; namely, information on IBD management, information on
medication use, additional information on IBD and uncontrolled symptoms
associated with IBD (Table 5).
Table 5. Pharmacists’ responses regarding the healthcare professional
best-suited for managing patients with IBD (n= 52)
|
Variable
|
Frequency (%)
|
|
To whom would the patient go for information about
managing their IBD?
|
|
General practitioner
|
39 (75.0)
|
|
Nursing support
|
1 (1.9)
|
|
Dietitian
|
10 (19.2)
|
|
Pharmacist
|
2 (3.9)
|
|
To whom would the patient go to for information about
medications for their IBD?
|
|
General practitioner
|
4 (7.7)
|
|
Dietitian
|
1 (1.9)
|
|
Pharmacist
|
47 (90.4)
|
|
To whom would the patient go to for
additional/supportive information about their IBD?
|
|
General practitioner
|
14 (26.9)
|
|
Nursing support
|
8 (15.5)
|
|
Dietitian
|
11 (21.1)
|
|
Pharmacist
|
17 (32.7)
|
|
Psychologist
|
2 (3.8)
|
|
Who would the patient see when their IBD symptoms are
not well controlled?
|
|
General practitioner
|
47 (90.4)
|
|
Nursing support
|
1 (1.9)
|
|
Dietitian
|
3 (5.8)
|
|
Pharmacist
|
1 (1.92)
|
IBD = Inflammatory Bowel Disease.
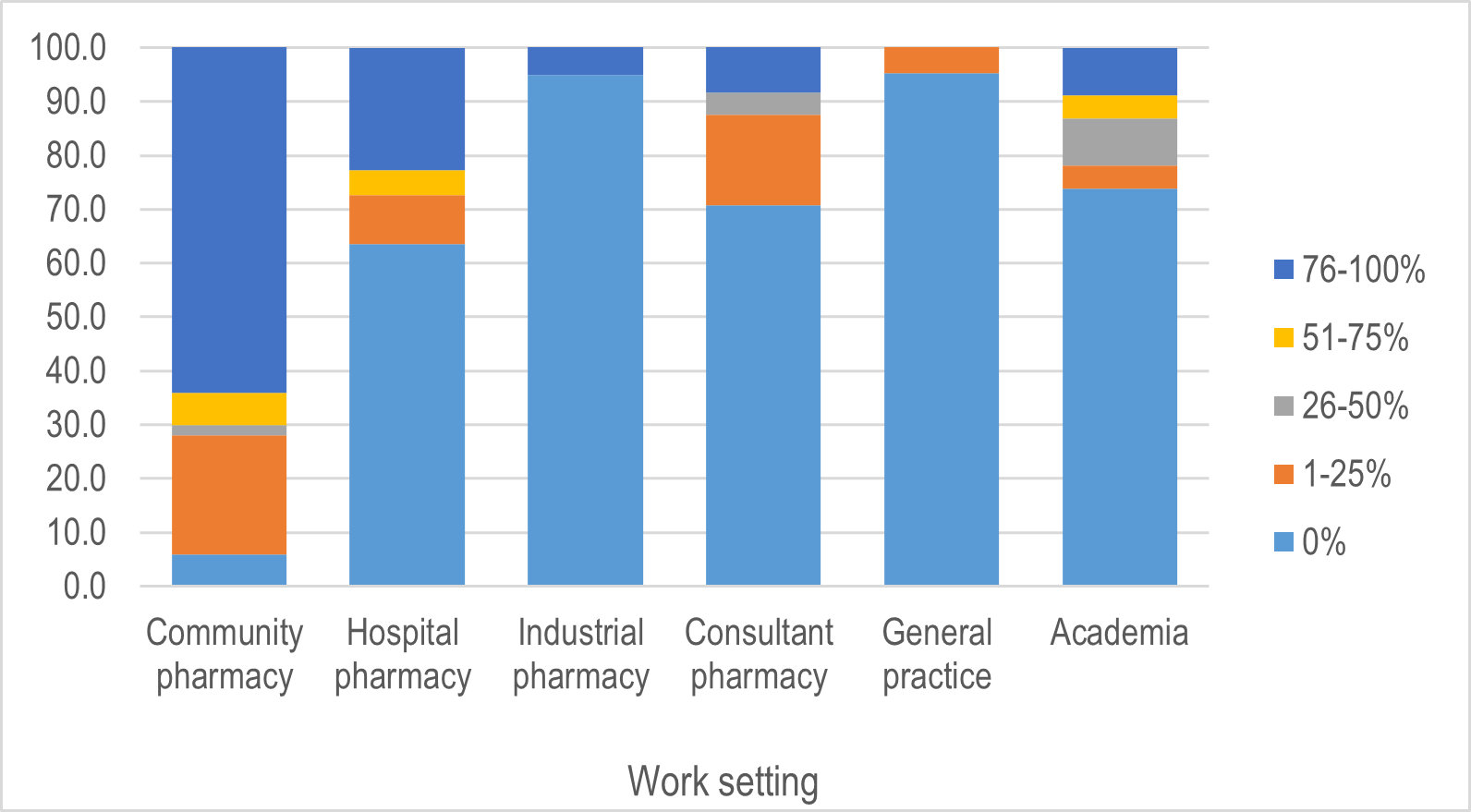
Pharmacists perceived GPs as the most important and psychologists as the
least important healthcare professionals in managing patients with IBD. For
providing information to patients about managing their IBD, GPs were
considered to be the most important (75%), followed by dietitians (19.2%),
pharmacists (3.9%), nursing support (1.9%) and then psychologists (0%).
Pharmacists were considered most important (90.4%) for patients seeking
medication information. When providing additional or supportive
information, all five healthcare professionals were perceived to have some
importance (32.7% for pharmacists, 26.0% for GPs, 21.1% for dietitians,
15.5% for nursing support and 3.8% for psychologists). For uncontrolled
symptoms of IBD, GPs were the most important healthcare professional group
(90.4%), and psychologists (0%) were the least important. Overall,
pharmacists ranked GPs as the most important healthcare professional in
managing patients with IBD, followed by pharmacists, dietitians, nursing
support and psychologists (Figure 2).
Figure 2. Ranking of pharmacists’ perception on the healthcare professional
best-suited in managing patients with IBD.

DISCUSSION
To the best of our knowledge, this is the first survey of pharmacists’
knowledge and perceptions of IBD management to be performed in Australia.
It contributes to filling a gap in the literature by exploring pharmacists’
role in managing IBD in a primary care setting. As IBD is a chronic disease
associated with high levels of morbidity and mortality, ongoing long-term
management is essential (Andrews et al. 2010). Therefore, pharmacists are
responsible for taking a prominent and proactive role in caring for
patients with IBD (Prasad, Duncanson et al. 2020). An adequate level of
knowledge can help pharmacists to understand the needs of patients with IBD
and be able to address them (Blackburn et al. 2019; Zezos & Panisko
2018), such as regular monitoring for adverse effects, management of
complex medication regimens, ensuring appropriate use of medications and
lifestyle education and support (Massuger et al. 2019; Strohl et al. 2018).
Our findings suggest that pharmacists had a low to moderate knowledge about
managing patients with IBD. Pharmacists demonstrated a high knowledge of
general concepts of IBD, but lower knowledge related to specific, advanced
IBD management concepts. The latter included low knowledge in colon cancer
screening, associated risk with smoking in IBD, the prevalence of IBD,
extraintestinal complications associated with IBD and vitamin deficiencies.
In addition, pharmacists also demonstrated a low level of knowledge about
medication-related aspects of care, such as OTC medication use leading to
toxic megacolon and place in therapy of biologics when treating IBD
patients. This suggests that pharmacists’ base their level of understanding
of IBD management as limited and highlights a gap in knowledge where more
comprehensive education is required (Prasad, Keely et al. 2020). While
knowledge can indeed be improved through educational sessions, there are
still potential barriers (such as limited available time, and access to
resources and guidelines), that require consideration for applicability in
practice (Blackburn et al. 2019; Tan et al. 2012; Zezos & Panisko
2018).
Compared with the national data, the distribution of gender and
registration by age group for pharmacists in Australia are consistent with
the statistics provided by the Pharmacy Board for the period ending June
2020. There were more female pharmacists compared to males and relatively a
similar proportion of pharmacists among all age groups except those aged
≤24 years. The findings also indicate that pharmacists perceived themselves
as having better knowledge about IBD prior to completing the knowledge
section of the survey. As demonstrated by Carvajal and colleagues, in a
sample of 1,000 pharmacists, the authors reported that gender and age group
classification influenced patterns of knowledge and how pharmacists applied
that knowledge in practice, such as the utilisation of drug information
resources (Carvajal et al. 2013). While there is sufficient evidence in
literature relating to professional education associated with improved
quality in healthcare, many only focus on the educational approach and
content (Love, Messman & Merritt 2019; The Health Foundation UK 2012).
There is a lack of evidence assessing the effectiveness of such educational
interventions regarding the impact of such education on patient health
outcomes or the long-term outcomes for patients and healthcare
professionals (The Health Foundation UK 2012).
Active learning strategies, such as experiential learning where experiences
and observations are conceptualised into practice, have shown to be more
effective as they allow for hands-on practice and reflection (Chamane,
Kuupiel & Mashamba-Thompson 2019; Lavallee et al. 2021; The Health
Foundation UK 2012). Pharmacists are responsible for their own
self-directed learning and maintaining continuing professional development
as part of their professional practice. In a more recent study, Prasad,
Keely et al. (2020) reported the confidence level of pharmacists before and
after an educational session on IBD and found that while pharmacists were
not confident managing patients with IBD, they expressed their willingness
to learn more about the disease. These results support the findings of the
current study and highlight that pharmacists’ knowledge of IBD is
suboptimal, therefore suggesting that there is a need to acquire and/or
update IBD-specific knowledge through continued education to improve
knowledge or enhance experience and management skills (Mikocka-Walus et al.
2014; Tan et al. 2012).
The deficit in their knowledge can be understood through the concept of
‘you don’t know what you don’t know’, which is an important consideration
in the context of any pre-/post-evaluation, and the application is relevant
to a range of diseases (McGregor 2004). For instance, the recent issue
surrounding the current COVID-19 pandemic, where little was known and still
unknown regarding managing the virus. To better our understanding, more
research and self-directed learning are needed to equip all healthcare
professionals supporting the community and the healthcare system. In
managing IBD, it is only through an accurate self-assessment that
pharmacists can identify and explore areas in which they require additional
learning. This difference between their perceptions of what they know and
the level of their IBD knowledge could be due to a degree of overconfidence
(Karpen 2018; Kovacs, Lagarde & Cairns 2020), limited experience with
IBD patients or misconception of IBD management (Prasad, Keely et al. 2020;
Tan et al. 2012). In addition, it is notable that the study also
demonstrated a statistically significant difference in knowledge scores
between pharmacists with exposure to IBD patients and those without. This
suggests that pharmacists require adequate exposure and familiarity with
IBD in their day-to-day practice to establish or enhance and maintain a
strong core knowledge and skills related to IBD management (Mikocka-Walus
et al. 2014; Tan et al. 2012). This is not surprising, as evidence
literature acknowledges that educational interventions alone are not likely
to generate improved quality of care in practice (The Health Foundation UK
2012). Therefore, it is more likely that regular interactions with people
living with IBD would drive self-directed learning among pharmacists,
contributing to their professional development and practices. Due to a
relatively smaller prevalence of 0.4% for IBD (Deloitte Access Economics
Pty Limited 2007; PricewaterhouseCoopers Australia 2013) when compared to
other chronic diseases such asthma and diabetes (Australian Bureau of
Statistics 2018; Australian Institute of Health and Welfare 2018),
pharmacists may provide advice to only a few IBD patients as part of their
everyday practice. This may reduce the clinical exposure necessary for
adequate knowledge and experience that is essential for optimal IBD
management (Tan et al. 2012).
Our study also explored pharmasists’ perceptions of the role of healthcare
professionals in primary care managing patients with IBD. Our findings
indicate that pharmacists consider GPs the key care provider for patients
with IBD in primary care. This supports current literature that suggests
that in Australia, most of out-of-hospital care for IBD patients is
delivered by GPs (Crohn’s & Colitis Australia 2017; Louis et al. 2015).
However, pharmacists perceived themselves as the key healthcare
professionals when providing information about medications to IBD patients.
This is highlighted extensively in published literature and supports the
role of pharmacists within a multidisciplinary care providing tailored
information to patients in chronic disease management (George et al. 2010;
International Pharmaceutical Federation 2019; Pharmaceutical Society of
Australia 2019). While dietitians and nursing support were considered to
have a role in managing patients, pharmacists perceived psychologists as
having no role in the management of IBD. This discovery was notable, given
the high burden of mental illness in IBD patients (Mikocka-Walus et al.
2020). While it would be noteworthy to explore why psychologists were
considered least important by pharmacists, this was not possible within the
scope of the study. As outlined in the current Australian IBD Standards, an
ideal IBD team should involve gastroenterologists, surgeons, nurses,
dietitians, psychologists, pathologists, radiologists and pharmacists
(Crohn’s & Colitis Australia 2016); however, GPs were not considered an
equally integral part of an ideal team (Crohn’s & Colitis Australia
2016; Prasad, Potter et al. 2020).
Multidisciplinary care is considered essential to IBD management but is
rarely implemented in practice (Koltun 2017; Lee & Melmed 2017; Ricci,
Lanzarotto & Lanzini 2008). The need for healthcare professionals
managing patients with IBD extends beyond the initial diagnosis stage to a
lifelong requirement (Louis et al. 2015). The addition of new therapies,
the approach of treat-to-target (shift from symptom control to mucosal
healing) and a change to a more patient-centred approach has all led to a
more challenging and involved role for healthcare professionals in the
management of IBD (Colombel et al. 2020). Pharmacists are trained and
qualified to provide the required care around medication management in a
primary care setting (International Pharmaceutical Federation 2019;
Pharmaceutical Society of Australia 2019) and have clearly demonstrated
their ability in other chronic diseases such as asthma and diabetes
(Prasad, Duncanson et al. 2020). In IBD, pharmacists have the opportunity
to acquire additional clinical skills and apply their knowledge and
expertise through primary care services to their patients in collaboration
with GPs and other healthcare professionals such as gastroenterologists and
IBD nurses (Massuger et al. 2019; PricewaterhouseCoopers Australia 2013).
This exploratory study provides valuable insights into factors that
contribute to the varying degree of knowledge among pharmacists working in
a primary care setting. The study was limited by a relatively small sample
size, cross-sectional design and online delivery method of the survey.
Firstly, data to calculate the number of registered pharmacists working in
a primary care setting was not available at the time of the study. Despite
efforts to collect data about a participant’s principal place of practice
by postcode, and because pharmacists may be employed in more than one
location, the information collected by the Australian Health Practitioner
Regulation Agency (Ahpra) was insufficient for the needs of this study.
Secondly, due to the anonymity of the survey, it was not possible to
identify the number of pharmacists who chose not to complete the survey and
determination of a response rate was not possible. Thirdly, the online
delivery may suggest that those who prefer electronic methods may be more
receptive to participating. Another limitation could be related to
pharmacists’ interest in the survey research topic. As IBD can be
considered a silent disease of small prevalence in comparison to other
chronic diseases, pharmacists may not have enough patients with IBD to
warrant awareness or understanding of IBD management. Based on the leverage
salience theory, the survey topic is one of the most important factors that
influence response rates (Groves, Singer & Corning 2000). In addition,
incentives have been used in some studies to motivate survey participation
in forms of monetary compensation (such as gift cards) and can be
considered a constraint of this study, as we did not offer any incentives.
For this study, we only included pharmacists who were working in a primary
care setting; therefore, the sample is unrepresentative of all Australian
pharmacists. Further, the global COVID-19 pandemic may have added to the
increased workload limiting available time for pharmacists to participate
in the survey, nor could we plan for alternative recruitment strategies.
Given all these possible limitations, the sample size limits inferences
associated with the study outcomes, with likely Type II errors. Like any
survey design, there is possible participation and self-reporting bias. As
this was an Australian study, it limits the generalisability of results to
other countries regarding IBD knowledge.
CONCLUSION
Despite the incidence and prevalence of IBD increasing globally, there are
few studies evaluating knowledge and perceptions of healthcare
professionals, especially pharmacists in primary care. Such studies are
important to allow for the adoption of proactive approaches that can
deliver appropriate and evidence-based care to people living with IBD. This
study indicates that the limited exposure to patients with IBD is directly
associated with pharmacists’ suboptimal knowledge managing IBD. As
healthcare professionals, pharmacists have a responsibility to update and
increase their knowledge of IBD. The ideal positioning of primary care
pharmacists to support people with IBD could be capitalised on with access
to a comprehensive educational response such as a specialty training
pathway. Educational interventions to improve understanding of treatment
options and the availability of accessible resources suited to primary care
management of IBD are potential opportunities for targeting this knowledge
gap. With high practical and translational implications, future research
could focus on whether educational interventions can improve and/or
maintain pharmacists’ knowledge and perception in managing IBD.
Funding
The authors received no financial support for the research, authorship,
and/or publication of this article.
Conflict of interest
The authors declare that there is no conflict of interest.
Abbreviations
IBD = Inflammatory bowel disease; GP(s) = General practitioners; OTC =
Over-the-counter.
Ethical Statement
The Research Ethics Committee approved the study protocolee at Hunter New
England Health [2019/ETH00167] and the University of Newcastle Human
Research Ethics Committee (HREC) [H-2019-0201].
References
Andrews, JM, Mountifield, RE, Van Langenberg, DR, Bampton PA &
Holtmann, GJ 2010, ‘Un-promoted issues in inflammatory bowel disease:
opportunities to optimize care’, Intern Med J, vol. 40, no. 3, pp.
173–182, viewed (4 Dec 2020), doi:10.1111/j.1445-5994.2009.02110.x.
Australian Bureau of Statistics 2018, Asthma - National Health Survey: First Results, 2017-18, cat. no.
4364.0.55.001, ABS, Canberra, viewed 19 May 2019,
https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release
Australian Institute of Health and Welfare (AIHW) 2018, Australia’s health 2018, cat. no. AUS 221, AIHW, Canberra, viewed
19 May 2019,
https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents
Bennett, AL, Munkholm, P & Andrews, JM 2015, ‘Tools for primary care
management of inflammatory bowel disease: do they exist?’, World J Gastroenterol, vol. 21, no. 15, pp. 4457–4465, viewed (4
Dec 2020), doi:10.3748/wjg.v21.i15.4457.
Blackburn, DF, Fowler, S, Crawley, A, Gerwing, S, Alcorn, J, Mansell, H,
Evans, C, Mansell, K, Taylor, J, Jorgenson, D, Larocque, D, Rotter, T &
Shevchuk, Y 2019, ‘An advanced pharmacy practice experience for community
pharmacies based on a clinical intervention targeting patients with
inflammatory bowel disease’, Journal of Pharmacy Practice, vol.
34, no. 1, pp. 51–57, viewed (4 Dec 2020), doi:10.1177/0897190019857410.
Carvajal, MJ, Clauson, KA, Gershman, J & Polen, HH 2013, ‘Associations
of gender and age groups on the knowledge and use of drug information
resources by American pharmacists’, Pharmacy Practice, vol. 11,
no. 2, pp. 71–80, viewed (4 Dec 2020), doi:10.4321/s1886-36552013000200003.
Chamane, N, Kuupiel, D & Mashamba-Thompson, TP 2019, ‘Experiential
learning for primary healthcare workers in low- and middle-income
countries: a scoping review protocol’, Systematic Reviews, vol. 8,
no. 1, p. 123, viewed (4 Dec 2020), doi:10.1186/s13643-019-1040-6.
Charan, J & Biswas, T 2013, ‘How to calculate sample size for different
study designs in medical research?’, Indian J Psychol Med, vol.
35, no. 2, pp. 121–126, viewed (4 Dec 2020), doi:10.4103/0253-7176.116232.
Colombel, JF, D’Haens, G, Lee, WJ, Petersson, J & Panaccione, R 2020,
‘Outcomes and strategies to support a treat-to-target approach in
inflammatory bowel disease: a systematic review’, J Crohns Colitis
, vol. 14, no. 2, pp. 254–266, viewed (4 Dec 2020),
doi:10.1093/ecco-jcc/jjz131.
Crohn’s & Colitis Australia 2017,
Inflammtory Bowel Disease Audit - final report of the first audit of
the organisation and provision of IBD services in Australia 2016
, prepared by Crohn’s & Colitis Australia, CCA, Camberwell, viewed (19
Feb 2021),
https://www.crohnsandcolitis.com.au/ibdqoc/ibd-audit-report/
Crohn’s & Colitis Australia 2016,
Australian IBD Standards: Standards of healthcare for people with
inflammatory bowel disease in Australia
, prepared by Crohn’s & Colitis Australia, CCA, Camberwell, viewed (19
Feb 2021),
https://www.crohnsandcolitis.com.au/ibdqoc/australian-ibd-standards/
Crohn’s & Colitis Australia 2007, The economic costs of Crohn’s disease and ulcerative colitis,
prepared by Deloitte Access Economics Pty Limited, viewed (4 Dec 2020),
https://crohnsandcolitis.org.au/wp-content/uploads/2022/02/Deloitte-Access-Economics-Report.pdfGastroenterological
Society of Australia 2018,
Clinical update for general practitioners and physicians. Inflammatory
bowel disease. Fourth edition. Updated 2018
, prepared by Gastoenterological Society of Australia, GESA, Melbourne,
viewed (12 Jan 2021),
https://www.gesa.org.au/public/13/files/Education%20%26%20Resources/Clinical%20Practice%20Resources/IBD/2018_IBD_Clinical_Update_May_update.pdf
George, PP, Molina, JA, Cheah, J, Chan, SC & Lim, BP 2010, ‘The
evolving role of the community pharmacist in chronic disease management - a
literature review’, Ann Acad Med Singapore, vol. 39, no. 11, pp.
861–867.
Georgy, M, Negm, Y & El-Matary, W 2019, ‘Quality improvement in
healthcare for patients with inflammatory bowel disease’, Transl Pediatr, vol. 8, no. 1, pp. 77–82, viewed (4 Dec 2020),
doi:10.21037/tp.2019.01.02.
Groves, RM, Singer, E & Corning, A 2000, ‘Leverage-saliency theory of
survey participation: description and an illustration’, Public Opin Q, vol. 64, no. 3, pp. 299–308, viewed (4 Dec 2020),
doi:10.1086/317990.
International Pharmaceutical Federation 2019,
Beating non-communicable diseases in the community - The contributions
of pharmacists
, prepared by the International Pharmaceutical Federation, FIP, The
Netherlands, viewed (8 Mar 2021),
https://www.fip.org/files/fip/publications/NCDs/beating-ncds-in-the-community-the-contribution-of-pharmacists.pdf
Janzen, D, Fitzpatrick, K, Jensen, K & Suveges, L 2013, ‘Women in
pharmacy: a preliminary study of the attitudes and beliefs of pharmacy
students’, Canadian Pharmacists Journal / Revue des Pharmaciens du Canada,
vol. 146, no. 2, pp. 109–116, viewed (14 Dec 2020),
doi:10.1177/1715163513481323.
Karimi, N, Moore, AR, Lukin, A, Kanazaki, R, Williams, AJ & Connor S
2020, ‘Clinical communication in inflammatory bowel disease: a systematic
literature review protocol’, BMJ Open, vol. 10, no. 11, viewed (14
Dec 2020), doi:10.1136/bmjopen-2020-039503.
Karpen, SC 2018, ‘The social psychology of biased self-assessment’, American Journal of Pharmaceutical Education, vol. 82, no. 5,
viewed (14 Dec 2020), doi:10.5688/ajpe6299.
Koltun, WA 2017, ‘Better together: improved care of the IBD patient using
the multi-disciplinary IBD center’, Expert Rev Gastroenterol Hepatol, vol. 11, no. 6, pp. 491–493,
viewed (14 Dec 2020), doi:10.1080/17474124.2017.1309289.
Kovacs, RJ, Lagarde, M & Cairns, J 2020, ‘Overconfident health workers
provide lower quality healthcare’, Journal of Economic Psychology,
vol. 76, viewed (14 Dec 2020),
doi:https://doi.org/10.1016/j.joep.2019.102213.
Lavallee, J, Byrne-Davis, L, Weinman, J & Hart, J 2021, ‘Effective
working in health care’, in Reference Module in Neuroscience and
Biobehavioral Psychology, Elsevier, viewed (14 Dec 2020),
DOI:10.1016/B978-0-12-818697-8.00058-3
Lee, CK & Melmed, GY 2017, ‘Multidisciplinary team-based approaches to
IBD management: how might “one-stop shopping” work for complex IBD care?’, Am J Gastroenterol, vol. 112, no. 6, pp. 825–827, viewed (14 Dec
2020), doi:10.1038/ajg.2017.124.
Louis, E, Dotan, I, Ghosh, S, Mlynarsky, L, Reenaers, C & Schreiber, S
2015, ‘Optimising the Inflammatory Bowel Disease Unit to improve quality of
care: expert recommendations’, J Crohns Colitis, vol. 9, no. 8,
pp. 685–691, viewed (14 Dec 2020), doi:10.1093/ecco-jcc/jjv085.
Love, JN, Messman, AM & Merritt, C 2019, ‘Improving the learning
experience through evidence-based education’, The Western Journal of Emergency Medicine, vol. 20, no. 1, pp.
1–5, viewed (8 Mar 2021), doi:10.5811/westjem.2018.10.41320.
Manolakis, PG & Skelton, JB 2010, ‘Pharmacists’ contributions to
primary care in the United States collaborating to address unmet patient
care needs: the emerging role for pharmacists to address the shortage of
primary care providers’, American Journal of Pharmaceutical Education, vol. 74, no. 10, S7,
viewed (14 Dec 2020), doi:10.5688/aj7410s7.
Massuger, W, Moore, GTC, Andrews, JM, Kilkenny, MF, Reyneke, M, Knowles, S,
Purcell, L, Alex, G, Buckton, S, Page, AT, Stocks, N, Cameron, D,
Manglaviti, F & Pavli, P 2019, ‘Crohn’s & Colitis Australia
inflammatory bowel disease audit: measuring the quality of care in
Australia’, Internal Medicine Journal, vol. 49, no. 7, pp.
859–866, viewed (9 Mar 2021), doi:10.1111/imj.14187.
McGregor, S 2004, ‘Learning with Donald Rumsfeld - flexible learning: the
relevance and resonance of multiprofessional learning in primary care’, The British Journal of General Practice, vol. 54, no. 506, pp.
722–723.
Mikocka-Walus, A, Andrews, JM, Rampton, D, Goodhand, J, van der Woude, J
& Bernstein, CN 2014, ‘How can we improve models of care in
inflammatory bowel disease? An international survey of IBD health
professionals’, J Crohns Colitis, vol. 8, no. 12, pp. 1668–1674,
viewed (14 Dec 2020), doi:10.1016/j.crohns.2014.07.009.
Mikocka-Walus, A, Massuger, W, Knowles, SR, Moore, GT, Buckton, S, Connell,
W, Pavli, P, Raven, L & Andrews, JM 2020, ‘Psychological distress is
highly prevalent in inflammatory bowel disease: a survey of psychological
needs and attitudes’, JGH Open, vol. 4, no. 2, pp. 166–171, viewed
(2 Jun 2021), doi:10.1002/jgh3.12236.
Pharmaceutical Society of Australia 2019,
Pharmacists in 2023: For patients, for our profession, for Australia’s
health system
, prepared by the Pharmaceutical Society of Australia, PSA, Canberra,
viewed (9 Mar 2021),
https://www.psa.org.au/advocacy/working-for-our-profession/pharmacists-in-2023/
Pharmacy Board of Australia AHPRA 2020, Pharmacy Board of Australia - Registrant data, viewed (14 Dec
2020),
https://www.pharmacyboard.gov.au/about/statistics.aspx
Phillips, AW, Friedman, BT, Utrankar, A, Ta, AQ, Reddy, ST & Durning,
SJ 2017, ‘Surveys of health professions trainees: prevalence, response
rates, and predictive factors to guide researchers’, Academic Medicine, vol. 92, no. 2, pp. 222–228, viewed (14 Dec
2020), doi:10.1097/ACM.0000000000001334.
Prasad, SS, Duncanson, K, Keely, S, Talley, NJ, Kairuz, T, Holtmann, GJ,
Shah, A & Walker, MM 2020, ‘A role for primary care pharmacists in the
management of inflammatory bowel disease? Lessons from chronic disease: a
systematic review’, Pharmacy (Basel), vol. 8, no. 4, viewed (14
Dec 2020), doi:10.3390/pharmacy8040204.
Prasad, SS, Keely, S, Talley, NJ, Kairuz, T & Walker, MM 2020,
‘Pharmacists’ confidence in managing patients with inflammatory bowel
disease’, Pharmacy (Basel), vol. 8, no. 2, viewed (14 Dec 2020),
doi:10.3390/pharmacy8020068.
Prasad, SS, Potter, M, Keely, S, Talley, NJ, Walker, MM & Kairuz, T
2020, ‘Roles of healthcare professionals in the management of chronic
gastrointestinal diseases with a focus on primary care: a systematic
review’, JGH Open, vol. 4, no. 2, pp. 221–229, viewed (14 Dec
2020), doi:10.1002/jgh3.12235.
Crohn’s & Colitis Australia 2013, Improving inflammatory bowel disease care across Australia,
prepared by PricewaterhouseCoopers, PwC, (Australia), viewed (4 Dec 2020),
https://crohnsandcolitis.org.au/wp-content/uploads/2022/02/PwC-report-2013.pdf
Ricci, C, Lanzarotto, F & Lanzini, A 2008, ‘The multidisciplinary team
for management of inflammatory bowel diseases’,
Official Journal of the Italian Soceity of Gastroenterology and the
Italian Association for the Study of the Liver
, 40 Suppl 2, S285–288, viewed (14 Dec 2020),
doi:10.1016/S1590-8658(08)60539-3.
Strohl, M, Gonczi, L, Kurt, Z, Bessissow, T & Lakatos, PL 2018,
‘Quality of care in inflammatory bowel diseases: what is the best way to
better outcomes?’, World Journal of Gastroenterology, vol. 24, no.
22, pp. 2363–2372, viewed (17 Sep 2021), doi:10.3748/wjg.v24.i22.2363.
Tan, M, Holloway, RH, Lange, K & Andrews, JM 2012, ‘General
practitioners’ knowledge of and attitudes to inflammatory bowel disease’, Internal Medicine Journal, vol. 42, no. 7, pp. 801–807, viewed (17
Sep 2021), doi:10.1111/j.1445-5994.2011.02586.x.
The Department of Health 2013, National Primary Health Care Strategic Framework, prepared by the
Standing Council on Health, Canberra, viewed (17 Sep 2021),
https://extranet.who.int/nutrition/gina/sites/default/filesstore/AUS%202013%20National%20Primary%20Health%20Care%20Strategic%20Framework.pdf
The Health Foundation UK 2012, Quality improvement training for healthcare professionals,
prepared by the Health Foundation, London, viewed (17 Sep 2021),
https://www.health.org.uk/sites/default/files/QualityImprovementTrainingForHealthcareProfessionals.pdf
von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gotzsche, PC, Vandenbroucke,
JP & STROBE Initiative 2007, ‘The Strengthening the Reporting of
Observational Studies in Epidemiology (STROBE) statement: guidelines for
reporting observational studies’, Lancet, vol. 370, no. 9596, pp.
1453–1457, viewed (14 Dec 2020), doi:10.1016/S0140-6736(07)61602-X.
Zezos, P & Panisko, D 2018, ‘Web-based learning in inflammatory bowel
diseases: general truths and current specifics’, World Journal of Clinical Cases, vol. 6, no. 11, pp. 410–417, viewed (17 Sep 2021), doi:10.12998/wjcc.v6.i11.410.