Developing and evaluating a professional development plan pilot for doctors
in unaccredited posts: A pilot study
Jill Thistlethwaite 1, 2, Lara McGirr1, Toni Vial1
Abstract
Purpose
In Australia, doctors from their third-year post graduation who are not
on specialist training pathways frequently work in unaccredited posts
with varying amounts of education and support. In 2019, the New South
Wales Ministry of Health (NSW Health) and the Health Education and
Training Institute (HETI) agreed on a pilot process for these doctors
to develop a professional development plan (PDP). The pilot aimed to
implement the process and evaluate its feasibility and acceptability.
Methodology/approach
The process was piloted at four sites in 2021. The evaluation
methodology was informed by the non-adoption, abandonment and
challenges to scale-up, spread and sustainability (NASSS) framework
with data derived from site meetings, interviews with doctors in
unaccredited positions and PDP supervisors, and analysis of PDPs and
time required.
Findings
A total of 42 doctors undertook the PDP process, of whom 25 were
interviewed. Of the 28 supervisors recruited, 13 were interviewed.
Three sites reported successful implementation, with most doctors having
a PDP in progress. Despite challenges associated with the diversity of
the workforce and workplaces, all sites were supportive of the process
being rolled out with appropriate resourcing.
Research implications
The research findings indicated that embedding a PDP process more
widely across the state will be complex due to the diversity of the
workforce and clinical workplaces.
Practical implications
The PDP process, while acceptable and feasible, needs to adapt to local
circumstances, including the workforce, supervisory capacity and
experience, individual doctor needs and available resources.
Originality
The evaluation supports the need for a supported PDP process for
doctors in unaccredited positions.
Limitations
The findings may not be transferable to all NSW Health facilities or to
other states or territories. Doctors who consented to be interviewed
were more likely to be positive about the process than those who did
not. The study did not include a cost evaluation or explore
cost-effectiveness due to the short time frame.
Keywords: professional development plans; continuing professional
development; junior doctors; service registrars; education evaluation
1Health Education and Training Institute (HETI), NSW Health, St
Leonards, NSW 1590, Australia
2Faculty of Health, University of Technology Sydney
Corresponding author:Jill Thistlethwaite, Health Education
and Training Institute (HETI), NSW Health, 1 Reserve Road, St Leonards, NSW
1590, Australia,
[email protected]
,
[email protected]
Introduction
In New South Wales (NSW), Australia, doctors in their first two years after
graduation (postgraduate year [PGY] 1 and 2) are referred to as
prevocational and undertake an educational program with supervisory support.
Following this, doctors are typically either accepted into a vocational
specialist structured training program in accredited hospital posts or take
up an unaccredited position. In NSW, the former are referred to as
registrars, while the latter are known variously as career medical
officers, senior resident medical officers or unaccredited trainees. The
National Medical Workforce Strategy 2021-2031 refers to doctors in
unaccredited positions as service registrars (Australian Government
Department of Health 2021). The recent rise in the number of medical
students in Australia without a concomitant increase in training posts has
led to a rise in the number of service registrars. These include those who
plan to apply for a specialist training position, have left a training
program, are uncertain of their preferred career or have decided not to
enter specialist training. Service registrars may also be international
medical graduates.
Service registrars have historically worked long hours in public hospitals,
carrying out similar tasks to specialist registrars but without the same
levels of supervision, education and limits on overtime. The importance of
their contribution to healthcare is not always given the recognition and
respect it deserves by medical and other health professionals, and service
registrars are prone to exploitation (Australian Government Department of
Health 2021). Because of concerns about these doctors, in 2008, the NSW
Ministry of Health (NSW Health) established the Hospital Skills Program
(HSP) through its education organisation, the Health Education and Training
Institute (HETI). It was a flexible training and development program
designed to provide a structured set of learning outcomes in a set of HSP
modules, launched between 2010 and 2012. They were based on authentic
clinical contexts and included emergency medicine, aged care, mental
health, children's health, hospital medicine, women's health, addiction
medicine, rural medicine, sexual health and Aboriginal health. However,
uptake has been poor, partly because of its detail and lack of strategic
direction for its use. Moreover, the modules have not been updated in line
with clinical guidelines or practice over the last nine years. The HSP was
also intended to include a professional development process undertaken by
the local health districts (LHDs) in which the doctors were employed. This
process consisted of each HSP doctor formulating a learning plan, defined
as a set of learning outcomes based on their role and educational needs,
planned activities to achieve the outcomes and evidence of learning.
Evidence of learning incorporated work-based assessment (WBA), comprising
observation and evaluation of the doctors' performance during clinical
activities.
HETI was aware of considerable concerns about the practicalities of
implementing such a process across the state, particularly in accessing
appropriate training, supervision and review for doctors working without
consistent on-site supervision. In 2013, a pilot professional development
plan (PDP) process was undertaken at one hospital, which found that while
there was variability in the engagement of the doctors, the process was
considered valuable and could be modified for other areas of practice. An
essential factor for success was a positive supervisory relationship in
which supervisors acknowledged the educational and other needs of the
non-specialist doctors. However, the time and resources required for
arranging and completing WBA limited feasibility, and there were general
misconceptions about WBA. The pilot report recommended trialling the
process at more sites before a statewide rollout (Ozolins et al. 2014).
The HSP continued to provide funds for education for all doctors in
non-accredited posts in NSW based on their perceived needs. However, this
workforce is diverse, with unaccredited posts across multiple specialties
and locations. Education has not been tailored to individual needs and
career progression. The Australian media has published stories about these
doctors' heavy workload (Lindsay 2019; McKinnell 2019). In response, the
Australian Medical Association (AMA) of NSW, an independent body
representing the state's medical profession, reported that its council was
'concerned about the growing cohort of junior doctors working in
unaccredited registrar positions and believes that this is a waste of human
capital and may be affecting the provision of safe, high-quality patient
care' (AMA NSW 2019).
In 2018, HETI agreed that more support for PGY3 to PGY5 doctors in
non-accredited posts was required. These doctors would now be referred to as
hospital non-specialist program (HNSP) doctors. In 2019, an agreement was
reached to pilot a supported PDP process in the state. In addition, the MBA
announced that all registered medical practitioners, with a few exemptions,
must have a written and ongoing PDP from 1 January 2023 (Medical Board of
Australia 2021).
By definition, a PDP ('trainee' or 'learner' may be substituted for
'employee'):
gives an overview of the competencies the employee worked on in the past
and which competencies the employee is planning to work on in the future …
is composed by the employee himself … and is used as the basis for or to
structure the conversations with the supervisor or the coach, who provides
the employee with feedback and stimulates the employee's reflection.
(Beausaert et al. 2011, p. 236)
Before piloting, the process was widely discussed and developed with
stakeholders across NSW Health. The consensus was that the NSW PDP process
aims to support HNSP doctors in a continuous cycle of improvement and
learning by determining their current level of competence and performance
and facilitating the identification and achievement of learning outcomes
related to their specific needs and career plans. We identified
conversations with supervisors as an important part of the process. They
offered an opportunity for the HNSP doctors to reflect on the learning
needs for their current clinical roles, future roles and career aspirations
with their supervisors' guidance. The example template for the pilot
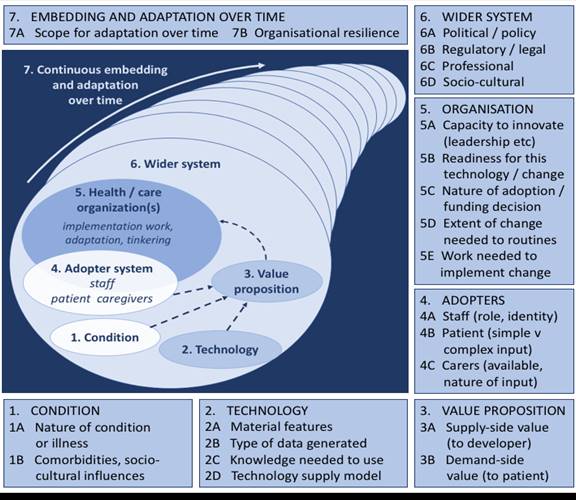
included the typical components of PDPs (Challis 2000), but these were not
mandatory. It was recommended that learning outcomes be written as
specific, measurable, achievable, realistic and timely (SMART) goals (Doran
1981). The supervisor's role included meeting with the HNSP doctor,
supporting the identification of learning goals and relevant learning
activities to meet the goals, discussing evidence of learning and advising
on career progression.
PURPOSE
The aims of the PDP pilot over 13 weeks were to develop, implement and
evaluate the process to enhance and sustain the training and satisfaction
of the HNSP workforce in NSW. The evaluation focused on the process's
feasibility and acceptability rather than longer-term outcomes such as
learning achievement, career development and patient outcomes.
METHODOLOGY AND APPROACH
The development and delivery of the HNSP require a change in management
approach. Greenhalgh and Papoutsi (2019) have described the dissemination
of innovation across a healthcare system as challenging but achievable by
considering three different logics of change and their underlying theories:
mechanistic (implementation science), ecological (complexity science) and
social (social science).
Implementation science focuses on the uptake of evidence-based practices
into routine practice (Nilsen 2015). In the case of the HNSP,
evidence-based education must inform the program. The intervention (the PDP
process) must be clearly defined and implemented, considering how individual
and organisational behaviour may be changed. Ideally, a small-scale trial in
a few settings is evaluated (i.e., a pilot process).
Complexity science studies complex systems that are uncertain,
unpredictable and emergent (Greenhalgh & Papoutsi 2019). Healthcare
settings are complex in nature and dependent on diverse groups of health
professionals, educators and administrators. To succeed in implementing the
HNSP, the unpredictability of the workplace and the need to modify the
program for local contexts must be recognised.
Social science aims to explore what people believe, why they work the way
they do, how they interpret others' actions and what they draw on to
achieve their (or a program's) goals. Staff work differently in different
contexts; they work around problems in diverse ways and adapt innovations to
their needs and resources. Thus, attempting to standardise a program as a
rigid 'one size fits all' model is unlikely to be feasible or acceptable.
These three approaches informed the methods of implementation and data
collection to capture the contextual factors underlying the adoption of the
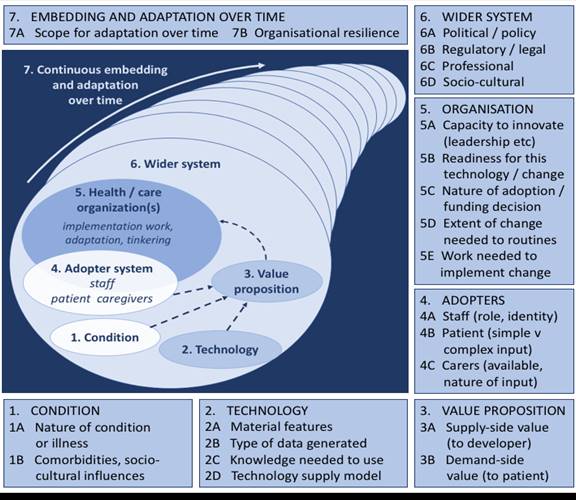
HNSP pilot PDP process. The framework for the evaluation was the
non-adoption, abandonment and challenges to scale-up, spread and
sustainability (NASSS) framework of Greenhalgh et al. (2017) (Figure 1).
The NASSS framework was developed as an evidence-based, theory-informed and
pragmatic framework to help predict and evaluate the success of
implementing a new technology-supported health or social care program. We
considered it appropriate for predicting and evaluating the implementation
of other programs - in this case, the PDP process for the HNSP. The
adoption and diffusion of innovations are not solely affected by individual
factors such as finance, technology, staff and learners considered
separately but by the dynamic interactions between them. It is these
interactions that were explored in the pilot. The seven domains of the
NASSS informed the evaluation of the pilot to help predict the feasibility
of the process and provide recommendations to enhance the likelihood of
adoption, given the current climate of doctor shortages and increased
workload pressures due to the ongoing COVID-19 pandemic. The pilot
evaluation questions are listed in Table 1.
Figure 1: The NASSS framework
Source: Greenhalgh T, Wherton J, Papoutsi C et al, 2017, 'Beyond adoption:
A new framework for theorizing and evaluating nonadoption, abandonment, and
challenges to the scale-up, spread and sustainability of health and care
technologies', J Med Internet Res, vol. 19(11): e367. doi:
10.2196/jmir.8775.
Published (and can be reproduced) under the terms of Creative Commons
Attribution 4.0 licence.
Table 1: Evaluation questions informed by the NASSS domains
|
|
Domain
|
Questions
|
|
1
|
Condition
(Lack of structure and support for the hospital
non-specialist medical workforce)
|
How is this condition perceived by participants?
What are the socio-cultural factors to consider in this
context?
|
|
2
|
Innovation (intervention)
(The professional development process)
|
What are the important features of the process?
What is required in terms of technology?
What knowledge and skills are needed to take part?
|
|
3
|
Value proposition
|
What is the business case/rationale for implementation?
What are the desirable outcomes, the effectiveness and
cost-effectiveness of the process?
|
|
4
|
The adopter system
|
What changes are implied for staff (HNSP doctors,
supervisors, support staff)?
What is expected of these individuals?
|
|
5
|
The healthcare organisation
|
How does the structure of the organisation (NSW Health) in
each local context affect the capacity to implement?
How ready is it for change?
What are the implications for the wider health team?
What work is needed to implement?
|
|
6
|
The wider system
|
What is the political and policy context underpinning the
implementation?
What are the regulatory or legal hurdles?
What inter-organisational work is required?
|
|
7
|
Embedding and adaptation
|
Is this process likely to be sustainable?
What affects the likelihood of sustainability?
What differences might be expected in different locations?
|
During the planning and implementation phases of the pilot, we used
appropriate evaluation methods to determine whether the domains were
simple, complicated or complex, as defined in the NASSS framework. A domain
is simple if it is straightforward and predictable, complicated if it has
multiple interacting components or issues and complex if it is dynamic and
unpredictable: 'The more complex an innovation or the setting in which it is
introduced, the less likely it is to be successfully adopted, scaled up,
spread, and sustained' (Greenhalgh et al. 2017).
ETHICAL APPROVAL
Hunter New England Research Ethics Committee provided ethical approval for
this project (2019/PID15113). Site-specific permission was also given.
SETTINGS AND PARTICIPANTS
Information on the pilot was shared with LHD chief executives. Expressions
of interest were invited towards the end of 2020, and the panel selected
four sites including metropolitan and rural areas. Funding was provided for
a clinical lead and an administrator at each site, who were responsible for
selecting and inviting HNSP doctors and supervisors to take part. We
provided resources including guides for HNSP doctors and supervisors and
the example PDP template (Figure 2), although we advised that other PDP
formats could be used.
Figure 2: The suggested PDP template
|
|
Examples
|
|
Date
|
|
|
Learning outcome(s)
SMART (specific, measurable, achievable, realistic and
timely)
|
|
|
Rationale: why do I need to achieve this outcome?
How do I know I need to achieve this outcome?
How will this improve my performance?
|
New post
Patient's unmet needs
Significant event audit
Supervisor advice
Review and planning meeting
Interest
Relevant college curriculum
Career intentions
|
|
How will I achieve this outcome?
How will I learn?
Activities
|
Online learning
Reading
Workshop
Departmental education
Observation and feedback
Practice
Paid course
|
|
Date achieved (partial/full)
|
|
|
What have I learned?
|
|
|
How do I know I have learned?
Evidence of learning
|
Formal certificate/assessment
Observation in practice such as mini-clinical evaluation
exercise, direct observation of practical skills,
multi-source feedback,
self-assessment
supervisor feedback
|
|
Current post
Application to current post
|
|
Data collection
The pilot process began in January 2021 and lasted 13 weeks (one term). A
wide range of data were collected during the pilot and in the following
weeks from:
- transcripts of Zoom meetings with pilot sites and the steering committee
- copies of PDPs
- supervisor and administration staff time logs
- transcripts of one-to-one Zoom interviews with supervisors and HNSP doctors
- end-of-pilot reports from each site.
Interviews were semi-structured with areas for discussion based on the
NASSS framework domains (Figure 1). They were iterative in that additional
topics were informed by analysis of previous interviews. Questions for
further exploration also arose during the interviews themselves. Interviews
lasted from 20 to 45 minutes and were conducted by the lead author.
Data analysis
Interview transcripts were analysed, synthesised and organised under the
seven domains of the NASSS framework. Content analysis (Liamputtong 2020)
was suitable for this study as it was not designed to develop new knowledge
but to evaluate the feasibility and acceptability of the PDP process,
describe the implications of the findings and develop recommendations for
NSW Health. Thus, there were specific questions the text needed to answer.
The study looked for patterns in the data rather than quantifying
responses. Data were analysed in Taguette, a basic qualitative data
software package. The content of the PDPs was quantified and described
according to the suggested areas to be included in the plans. Quantitative
data were extracted from time logs and reports and tabulated.
Findings
Of the 42 HNSP doctors who undertook the PDP process, 25 were interviewed.
Two additional HNSP doctors at Site C who were not in the pilot were
interviewed for comparison. Two at Site D who were not allocated a
supervisor to start the process in time were also interviewed. Of the 28
supervisors who participated, 13 were interviewed (Table 2). This
convenience sample was drawn from participants who responded to our
invitation, signed a consent form and were available to be interviewed
during the evaluation period. The study analysed 31 PDPs and all time logs
from each site. Three of the pilot sites reported successful implementation
of the PDP process with good engagement by HNSP doctors and supervisors.
The team at Site D, two hospitals in a rural and remote area, was delayed
in recruiting staff to the pilot director and administrator positions. This
led to late dissemination of information about the pilot to hospital staff,
including HNSP doctors, and no orientation event at the start of the term,
resulting in minimal uptake of the process. The PDPs contained from two to
30 learning outcomes; eight had SMART goals.
Table 2: Four pilot sites and participant data
|
Site
|
A
|
B
|
C
|
D
|
|
Description
|
New critical care rotation with 15 HNSP positions in one
district metropolitan hospital
|
HNSP doctors in different departments in one major
metropolitan teaching hospital
|
LHD with four hospitals involved, HNSP doctors in intensive
care unit and emergency departments
|
Rural and remote LHD with two hospitals involved and
multiple departments
|
|
Number of HNSP pilot doctors
|
14
|
18
|
19
|
20**
|
|
Interviewed
|
8
|
7
|
9 + 2*
|
3
|
|
Number of pilot supervisors
|
10
|
14
|
4
|
|
|
Interviewed
|
3
|
3
|
3
|
4
|
*At Site C, nine HNSP doctors in the pilot were interviewed and two HNSP
doctors not in the pilot were interviewed to compare.
**At Site D, there were 20 eligible HNSP doctors, only one of whom started
a PDP with supervisor support. Three HNSP doctors and four potential
supervisors were interviewed.
Participants' quotations are identified by the site letter (A, B, C or D),
followed by 'S' for supervisors or a PGY number for HNSP doctors. For
example, BS006 indicates a supervisor at Site B, and B3009 indicates a PGY3
HNSP doctor at Site B.
DOMAIN 1: THE CONDITION
The nature of the condition is a lack of structure and support for service
registrars, compared to doctors on specialist training programs.
So, their progress is not really tracked or measured, and they often don't
get much feedback in terms of where they are compared to their colleagues
and what's expected of them and what they can do to improve. (BS004)
I don't think I expected [in PGY3] to feel quite so unguided as to what to
study or what to work on. (A4005)
The diversity of the individuals within this group is high, adding to the
complexity of the condition. The pilot cohort included graduates from nine
Australian medical schools and international medical graduates from
countries including the United Kingdom, China, Pakistan, India, Nigeria and
Brazil. The HNSP doctors reported varying levels of support depending on
their department, the number of trainees, the availability of supervisors
or mentors and their working rotas.
DOMAIN 2: INNOVATION AND TECHNOLOGY
While the intervention (the PDP process and documentation) is not
innovative in its conception or adoption in many settings, including
healthcare, it is novel for this cohort. Many interviewed reported having
no experience setting their own learning goals or developing individualised
learning plans or PDPs. PGY4 doctors and above were more likely to report
self-directed learning experience, either individually or facilitated.
Not like this where you meet with someone more experienced to help and
really organises [sic] a plan. Of course, we all make plans in our minds,
but that's different. So, I haven't had one before. No. (C3019)
I think I've done them before but not for a whole year, it's more just like
as a junior doctor, you often work in terms of 10 weeks. Quite a few times
at the start of 10 weeks, if your consultant has time, they'll sit down and
be like, what do you want to get out of this term? So yeah, I think I have
done them before but they're quite informal. (D3001)
Interview data strongly indicate that a timely orientation package is
required to brief and support HNSP doctors before starting a PDP.
Supervisors offered differing levels of support depending on each doctor's
engagement with the process and ability to set, monitor and provide
evidence of learning.
They were, I mean even when we introduced the PDPs at our orientation day,
they said well who's going to give that to us … [we said] no, this is your
chance to develop it yourself. (AS015)
Site A recommended that HNSP doctors use the My Osler application for PDP
development (https://www.oslertechnology.com) and site B used Microsoft
Teams rather than the paper-based template. While My Osler was well liked,
particularly due to its portability, Microsoft Teams was found clunky and
hard to master. Interviewees identified what a suitable platform needed.
Easily accessible by everybody. Functional. Not so many buzzwords, just
really down-to-earth, simple type of stuff where you can document your
roles, your plans and your outcomes and whether you achieve it. I think
that's all you need. (BS006)
DOMAIN 3: THE VALUE PROPOSITION
The aim of supporting HNSP doctors is to improve patient outcomes and
safety by realising the full potential of each doctor in the NSW Health
system. It will be difficult to show a direct link between the introduction
of the PDP process and patient care without an in-depth long-term
evaluation. Thus, the return on investment is difficult to measure.
However, support for doctors is likely to improve performance, and the
doctors in the pilot had positive feedback about the process and its
necessity. The value will need to be clear to all, including funders and
all staff, prior to statewide adoption, which highlights the importance of
advertising the benefits of the process. These were identified as support,
structure, development guidance, career advice, mentoring and enhanced
wellbeing.
I think a big positive is actually seeing - keeping a record of it,
actually seeing the work you're putting [in] and what you're achieving.
Because I think I've always done things before but never really recorded it
and so never really felt like I was accomplishing anything. So, I think
it's positive reinforcement when you see what you're accomplishing, you
feel more motivated to continue. (A4005)
They get something out of it from a career perspective, but I think they
also get something out of it from a wellbeing perspective. (CS001)
I do like that there's a bit more structure and the fact that the whole
department's aware that I'm trying to progress with something and I'm not
just trying to cruise through the year, and that's been really helpful.
(B3005)
For some, the PDP process was seen as of essential value in principle, but
problematic in practice, due to local difficulties with staffing levels and
the senior workforce having to take on additional supervisory tasks.
DOMAIN 4: THE ADOPTER SYSTEM
Most HNSP doctors stated that they would continue the process if support
was provided. However, expectations need to be realistic, and there could
be a danger of losing the educational value.
Yes. I think so. Absolutely. Especially because I feel that the
supervisors, they are willing to help any time (C3019)
I know I have a cynical view of top-down implemented programs because they
tend to turn into tick box exercises, or they add workload onto somebody
that doesn't really want the workload and you don't really get the
engagement in that type of implementation. (D6014)
The PDPs analysis indicated that HNSP doctors need support to recognise
learning goals and provide evidence of learning. Few PDPs included SMART
learning goals. Instead, goals were broad and vague, without a rationale or
timeline for achievement. Most goals were clinically focused, and few were
professional or career oriented. In addition to developing new skills in
self-directed learning, adopters will need to engage with feedback.
Differences were noted in the HNSP doctors' comfort levels in eliciting
feedback. This facet of learning needs addressing to help HNSP doctors set
learning goals and gain evidence of meeting them.
It would be very rare that I'd ask someone directly for feedback. (C3010)
I think I definitely go for feedback. Especially when something has gone
wrong, or I don't think I've done such a good job or I'm unsure about
things. (B4001)
I've had some feedback from my supervisors and I thought that was really
helpful. So, I've been asking people to tell me if I'm doing something
wrong or if I can do something better and what they think is going to help
me for future learning. (C3019)
It's really variable. Sometimes really well because their personal values
or approach encourages the seeking of feedback for them as an individual to
almost never and in the group of those who almost never seek it, I'm never
sure if it's just because they don't know that they can or if they're
afraid of what they may hear as well. (DS001)
The supervisors were positive about the process, but they recognised that
even in a pilot with supposedly engaged trainees, the response may be
variable. Some trainees would require extra input and workload. Supervisors
themselves could vary in enthusiasm, and sufficient time for training for
new supervisors would be required.
As a supervisor or as somebody who's trying to mentor these younger
doctors, you've got to want to do it, you've got to have some interest, and
you've got to show some enthusiasm. (AS001)
Some supervisors may feel that they don't have the skills to sit down and
talk to trainees about professional development. So, they might feel that
they need a bit of guidance in what it is they need to do. (AS005)
DOMAIN 5: THE ORGANISATION
The overall organisation is NSW Health, with multiple health districts and
hospitals. In the pilot, the organisation included the local hospitals at
the four sites. Within the organisation are clinical workplaces of diverse
sizes, geography and capacity to innovate. Taking all sites into account,
the organisation is complex. Participants at all pilot sites were highly
supportive of the PDP process, including Site D, even though the process
there did not run as envisaged due to communication issues. The PDP process
will not deliver short-term cost savings and requires resources to
introduce and support it. Local organisations will need to factor in time
for trainees and supervisors in a system where non-specialist trainees are
frequently used to fill gaps in work rotas.
In our team, the unaccrediteds typically do do more nights. (B4001)
At the time of being interviewed, most HNSP doctors at three sites had had
either one or two meetings with their supervisor. Some had a third meeting
planned. Sessions lasted from 15 minutes to one hour, with the first
meeting typically longer than the second. For supervisors, time was not only
spent in discussion but also on documentation and, outside meetings,
organising times to meet.
It's pretty hard to find the time. (B4001)
I've negotiated some non-clinical time to be able to do that. (AS001)
Time logs indicated that the PDP process would require a minimum of 1.5 to
three hours' clinical release time for a supervisor and each HNSP doctor
over a 13-week term, with variable additional time for documentation and
arranging meetings. Once embedded, administration should take less time than
the pilot process. Depending on the number of doctors per site, it could
require the equivalent of at least 0.125 full-time work (just over half a
day per week).
DOMAIN 6: THE WIDER SYSTEM AND CONTEXT
Most interviewees agreed that the PDP process should become mandatory.
I think it would have to be a top-down approach for all unaccredited
trainees in New South Wales, and probably for Australia, if I'm honest; but
to start with, New South Wales first. I don't think it can be hospital
specific. I think if you're going to have something like this, it should be
done for all trainees. (AS001)
I think it's still quite flexible and you can make it quite personal so no
[misgivings about being mandatory]. (D3001)
Some interviewees noted that not all departments and hospitals have
adequate staffing, particularly in rural areas. They are likely to struggle
with additional supervisory commitments, particularly as many potential PDP
supervisors are also supervising doctors on specialist training pathways
and have other teaching responsibilities.
Now you've got often non-accredited doctors who are actually most in need
of support and training working in areas that are least equipped to provide
the support and training. (DS003)
Both accredited and unaccredited trainees and even I have medical students
from [XX] Uni who come through. I supervise them as well. (BS001)
DOMAIN 7: EMBEDDING AND ADAPTATION OVER TIME
A new process will need to adapt to ensure its sustainability and to become
embedded in clinical practice. Building PDP requirements into contracts for
HNSP doctors and supervisors was seen as important for success.
For it to work, I feel like having a dedicated supervisor who has this
supervision part as a part of their non-clinical portfolio would be a good
thing. (CS001)
The pilot lasted one term, whereas the process, if embedded, would extend
at least three years (from PGY3 to PGY5) for the HNSP doctors. Ongoing
supervision will need to be considered as doctors move within the
organisation. It will be difficult for doctors to retain the same PDP
supervisor after changing location or department. Several doctors advocated
having the same supervisor for one year, while others saw the benefits of
change.
Keeping the same person is definitely better, to have that continuity, I
think, is really important. To move supervisors, which is something I did
in [XX], was frustrating, and always felt like you never really got to know
someone. (B4007)
Maybe it's a good idea to see someone else because they might have
different experiences and they might have different options. They might
know different courses, or they might know different people to help me
organise a meeting with someone from my specialty. It might be a good idea
to talk to someone with different experiences. I don't see that as a
problem. (C3019)
Discussion
The ongoing tension between the education of recently qualified doctors and
clinical service delivery is increasingly recognised. For example, among
other initiatives, the American Medical Association Accelerating Change in
Medical Education Consortium aims to create flexible, individualised
learning plans to optimise the healthcare learning environment (Andrews et
al. 2021). This pilot and the NSW PDP process have similar aims. The NASSS
analysis of the pilot data showed that adopting and embedding a supported
mandatory PDP process for HNSP doctors in NSW, while acceptable and
feasible, will be complex. This was expected, given the diversity of the
workforce, clinical workplaces and the overarching health system. The
complexity implies that the process rollout is likely to be unpredictable
in its adoption, dynamic and emergent (Greenhalgh et al. 2017).
Twenty-three recommendations for statewide implementation of the PDP process
arising from the pilot have been discussed with NSW Health. We have
recommended that the supervisor supported PDP process be mandatory. While
professional development may be more sustained if PDPs are voluntary (Smith
& Tillema 2001), PDPs are becoming mandatory in Australia in 2023 in
any event. If they are developed with supervisor input that addresses
learners' needs, they are less likely to be a tick box exercise, as many
mandatory activities become (Macdougall, Epstein & Highet 2017).
As with other transitions in healthcare, the addition of a PDP process for
HNSP doctors needs to be supported by a timely, statewide orientation that
includes the rationale for its implementation. Online resources for HNSP
doctors and supervisors are being developed. These explain the process,
show what a PDP should consist of and demonstrate examples of content. The
doctors should be supported to develop their learning goals with
supervisors' input. The focus of the process needs to be on the individual
doctor with facilitation tailored to their preferences (Jennings 2007),
career goals and experience. The required support level depends on each
doctor's experience with PDPs as medical students or prevocational doctors
(PGY1 and PGY2) and their comfort with feedback dialogues. Many
interviewees stated they had little to no experience setting learning goals
and variable experience in engaging with feedback. It is critical to avoid
the tensions that have arisen with the portfolio-based assessment of
students (Oudkerk Pool et al. 2020). The PDP process should be viewed as a
supportive activity for learning rather than an assessment so that doctors
are honest about their strengths and areas for improvement. Engaged doctors
should require less supervisory input as they progress, particularly if the
PDP process enhances their agency and ability to take advantage of a range
of work-based learning opportunities (Watling et al. 2021). This would give
supervisors more time to motivate non-adopters. Consideration will need to
be given to the time and resources required to train supervisors. An
ePortfolio may be advisable to develop and share PDPs, though these have
cost and security implications. In medical training, PDP portfolios may
have contrasting purposes in assessment and support (van der Gulden et al.
2022). In this process, the ePortfolio would have two goals related to
support: (1) monitoring and planning doctor development, and (2)
stimulating reflection (Driessen & van Tartwijk 2018). The lack of a
suitable technological platform that is supported statewide complicates the
adoption of the PDP process.
The process needs to be adaptable to local hospital and district
circumstances, such as workforce issues (particularly in rural and remote
areas), supervisory capacity and experience, individual HNSP doctors' needs
and availability of resources (hours and support). Significant time and
effort across the organisation are required to set up and document meetings
and find suitable times to meet. These factors may be mitigated by paid
additional administration support as provided in the current pilot.
Governance is also needed to ensure that doctors meet the PDP process
requirements.
STRENGTHS AND LIMITATIONS
A strength of the pilot evaluation is using the NASSS framework to inform
data collection and analysis. The study did not solely look at outcomes. It
also examined the development and implementation process and implications
for the wider rollout of the PDP process.
The pilot was undertaken at four sites. Almost half of the HNSP doctors
involved (excluding those at Site D) and 13 supervisors were interviewed.
The study also analysed PDPs and collected data on administration and
supervision time. This resulted in a sizeable amount of data to apply the
NASSS framework, make recommendations for the rollout and enhance
sustainability. However, due to the short length of the pilot (13 weeks), we
were unable to explore longer-term outcomes in terms of benefits for the
HNSP doctors and the health system.
The HNSP doctors and supervisors were recruited to the pilot following
successful expressions of interest by their LHDs. Those doctors who
consented to be interviewed were more likely to be positive about the
process than those who did not or the small number who withdrew or did not
engage with the PDP process. A late start and slow uptake hampered the
process at one site, but this experience informed the evaluation.
The findings of this evaluation may not be transferable to all NSW Health
facilities or other states and territories. However, within the applied
framework, they capture the complicated and complex nature of the HNSP
condition. This has informed significant recommendations that recognise
those complexities and how they may be mitigated.
Given the short time frame, we did not conduct a cost evaluation or explore
cost-effectiveness, apart from collecting data about supervisor and
administrative time required during the pilot. There need to be more
cost-related studies in professional health education, including continuing
professional development (Cook, Wilkinson & Foo 2022). This aspect of
the process will be more closely examined when it is implemented statewide.
Conclusion
The evaluation of the PDP process for doctors in unaccredited positions
indicates that the process is acceptable and feasible. However, it must
also be capable of adapting to local circumstances, including workforce,
supervisory capacity and experience, individual doctor needs and available
resources.
Note: PDPs are mandatory in Australia for all doctors (with a few
exceptions). At the time of this publication, this was dependent on
doctors having a CPD home, and there were no suitable CPD homes for
doctors in unaccredited positions. Therefore, the requirement to have a
PDP will not be enforced until 2024 for this group.
Acknowledgements
We want to thank all the doctors, supervisors and administrative support
staff who participated in this pilot.
Conflict of interest
The authors declare no conflicts of interest.
Funding
This pilot evaluation was funded by NSW Health and carried out by the authors as part of their regular
remunerated positions with HETI.
References
AMA NSW 2019, Protection for doctors-in-training, AMA, viewed 25
October 2022,
https://www.amansw.com.au/protections-for-doctors-in-training/
Andrews, JS, Lomis, KD, Richardson, JA, Hammoud, MM & Skochelak, SE
2021, 'Expanding innovation from undergraduate to graduate medical
education: A path of continuous professional development',
Medical Teacher
, vol. 43, sup. 2, pp. S49-S55.
https://doi.org/10.1080/0142159X.2021.1935835
Australian Government Department of Health 2021,
National Medical Workforce Strategy 2021-2031
. Australian Government Department of Health.
Beausaert, S, Segers, MR, van der Rijt, J & Gijselaers, WH 2011, 'The
use of personal development plans (PDPs) in the workplace: A literature
review', in P van den Bossche, W Gijselaers & R Milter (eds),
Building learning experiences in a changing world
,Springer, Dordrecht.
Challis, M 2000, 'AMEE medical education guide no. 19: Personal learning
plans', Medical Teacher, vol. 22, no. 3, pp. 225-236.
Cook, DA, Wilkinson, JM & Foo, J 2022, 'Quality of cost evaluations of
physician continuous professional development: Systematic review of
reporting and methods', Perspectives on Medical Education, vol.
11, no. 1.
https://doi.org/10.1007/s40037-022-00705-z
Doran, GT 1981, 'There's a S.M.A.R.T. way to write management's goals and
objectives', Management Review, vol. 70, no. 11, pp.35-36.
Driessen, E & van Tartwijk, J 2018, 'Portfolios in personal and
professional development', in T Swanwick, B O'Brien & K Forrest (eds),
Understanding medical education, 2nd edn, Wiley, Oxford.
Greenhalgh, T & Papoutsi C 2019, 'Spreading and scaling up innovation
and improvement', British Medical Journal, vol. 365. 12068.
https://doi.org/10.1136/bmj.l2068
Greenhalgh, T, Wherton, J, Papoutsi, C, Lynch, L., Hughes, G., A'Court, C,
Hinder, S, Fahy, N, Procter, R & Shaw, S 2017, 'Beyond adoption: A new
framework for theorizing and evaluating nonadoption, abandonment, and
challenges to the scale-up, spread and sustainability of health and care
technologies', Journal of Medical Internet Research, vol. 19, no.
11.
https://doi.org/10.2196/jmir.8775
Jennings, SF 2007, 'Personal development plans and self-directed learning
for healthcare professionals: Are they evidence-based?'
Postgraduate Medical Journal
, vol. 83, pp. 518-524.
Liamputtong, P 2020, Qualitative research methods, Oxford
University Press, Docklands, Victoria.
Lindsay, T 2019, Time to end unaccredited registrar positions,
Insight+, viewed 25 October 2022,
https://insightplus.mja.com.au/2019/5/time-to-end-unaccredited-registrar-positions/
Macdougall, C, Epstein, M & Highet, L 2017, 'Continuing professional
development: Putting the learner back at the centre',
Archives of Disease in Children: Education and Practice
, vol. 102, pp. 249-253.
McKinnell, J 2019,
Sydney surgeon quits dream job after seeing 'the dark side' of the
profession
, ABC News, viewed 25 October 2022
https://www.abc.net.au/news/2019-02-06/sydney-surgeon-doctor-hours-unsw-yumiko-kadota-stress/10784238
Medical Board of Australia, AHPRA, 2021,
Registration standard: Continuing professional development
, Medical Board of Australia, Canberra.
Nilsen P 2015, 'Making sense of implementation theories, models and
frameworks', Implementation Science, vol. 10, p. 53.
https://doi.org/10.1186/s13012-015-0242-0
Oudkerk Pool, A, Jaarsma, ADC, Driessen, EW & Govaerts, MJB 2020,
'Student perspectives on competency-based portfolios: Does a portfolio
reflect their competence development?'
Perspectives on Medical Education
, vol. 9, pp. 166-172.
https://doi.org/10.1007/s40037-020-00571-7
Ozolins, I, Leslie, S, Greene, D & Vial, T 2014,
HSP professional development process pilot
, HETI, Sydney.
Smith, K & Tillema, H 2001, 'Long-term influences of portfolios on
professional development', Journal of Educational Research, vol.
45, pp. 183-202.
van der Gulden, R, Timmerman, A, Muris JWM, Thoonen, BPA, Heeneman, S &
Scherpbier-de-Haan, ND 2022, 'How does portfolio use affect self-regulated
learning in clinical workplace learning: What works, for whom and in what
contexts?', Perspectives on Medical Education, vol. 11, pp.
247-257.
https://doi.org/10.1007/s40037-022-00727-7
Watling, C, Ginsburg, S, LaDonna, K, Lingard, L & Field, E 2021, 'Going
against the grain: An exploration of agency in medical learning',
Medical Education
, vol. 55, pp. 942-950.
https://doi.org/10.1111/medu.14532