Online learning for allied health knowledge translation: A systematic review
Anna Joy
 1,2,
Leeanne M. Carey
1,2,
Leeanne M. Carey
 1,3,
Cheryl Neilson
1,3,
Cheryl Neilson
 4
, Kylee J. Lockwood
4
, Kylee J. Lockwood
 1,
Katherine E. Harding
1,
Katherine E. Harding
 1,5
1,5
Abstract
Purpose
To synthesise evidence on the effectiveness of online learning platforms for facilitating knowledge translation in allied health professionals.
Approach:A systematic review of the
literature searched three databases (Medline-OVID, CINAHL, Embase)
in November 2023 for studies measuring outcomes of knowledge
translation initiatives targeting allied health professionals
delivered using online learning platforms. Papers were eligible if
allied health professionals made up at least 50% of the sample,
most of the learning component was online, and comparative data was
reported. Data were extracted using a customised form. Quality of
studies was appraised using the Downs and Black checklist.
Meta-analyses were conducted where sufficient homogenous data were
available.
Findings:
Twenty-three studies published over a 13-year period were included
in this review primarily using pre-post study designs. All reported
improvements in either knowledge, skill and/or confidence, with an
meta-analysis (n=9 studies) showing a significant increase in
knowledge gain after exposure to online learning (SMD 1.39; 95% CI
= 0.96-1.83). However, there is little evidence that participation
in online learning is associated with a change in clinical practice.
Research implications:
This study supports previous research that online learning can
improve knowledge but highlights a need for more rigorous studies
addressing the impacts on behaviour change.
Practical Implications:
Online learning is an effective way of improving knowledge, skill
and/or confidence but additional knowledge translation strategies
may be needed to lead to a behaviour change.
Originality/value:
Synthesis of current knowledge of the value and limitations of
online learning as a tool to facilitate the implementation of
evidence into practice in the allied health professions.
Limitations:
This review was limited to studies published in the English
language only. The quality of studies in this field is low. Few
studies measure behaviour change.
Funding:
Funding support was provided by the National Health and Medical
Research Council. The protocol was registered with PROSPERO
(CRD42020147013).
Conflict of Interest:
No authors report a conflict of interest for this study.
Acknowledgements:
We acknowledge funding support from the National Health and Medical
Research Council (NHMRC) of Australia Partnership grant
(GNT1134495) and NHMRC Ideas grant (GNT2004443) awarded to LMC.
Keywords:Electronic learning, online learning, allied
health professionals, knowledge translation, behaviour change.
1 Occupational Therapy, School of Allied Health, Human
Services and Sport, La Trobe University, Bundoora, VIC 3086, Australia
2 School of Primary and Allied Health Care, Monash
University, Frankston, VIC 3199, Australia
3 Neurorehabilitation and Recovery, The Florey Institute of
Neuroscience and Mental Health, Melbourne Brain Centre, Austin Campus,
Heidelberg, VIC, 3084
4 Occupational Therapy, La Trobe Rural Health School, La
Trobe University, Bendigo, VIC, Australia
5 Eastern Health, Melbourne, Australia
Corresponding author: Anna Joy,
Occupational Therapy Department, Monash University Peninsula
Campus, Moorooduc Highway, Frankston, VIC 3199
, [email protected]
Introduction
The ability of healthcare workers to translate clinical practice
guidelines and research evidence into clinical practice is an important
component of knowledge translation. 1 Knowledge translation
has been defined as the exchange, synthesis and application of research
findings into practice. A recognition of the lengthy delays in
translation of knowledge into practice2-4 has
led to the emergence of implementation science as field of enquiry that
addresses questions of how interventions are adopted. 5 The
intended outcome of successful knowledge translation is an improvement
in the quality of patient care by increasing the provision of clinical
care that is informed by high quality clinical evidence. 6
For allied health professionals this not only requires the acquisition
of knowledge, skill and confidence, 7 but also a change in
behaviour.
Allied health practitioners encompass a range of healthcare
professional groups. While some definitions of allied health are broad,
incorporating professions such as pharmacy and medical imaging, a
narrower subgroup of allied health therapies has also been defined that
includes occupational therapists, physiotherapists, speech
pathologists, social workers, and dietitians all with a wide range of
evidence supporting their assessment and intervention practices.
8
In relation to use of evidence in practice, allied health professionals
share common issues with other members of the healthcare workforce,
such as medical and nursing professionals, but also have differences.
The type of evidence requiring translation often includes a focus on
delivery of complex interventions and optimising wellbeing through
prevention and recovery rather than diagnosis and cure, and allied
health professionals practise in a very diverse range of settings.
Although allied health professionals have an interest in using
evidence-informed practice previous studies have suggested that they
lack confidence in translating evidence into practice. 9
Barriers have been identified that impact the implementation of
evidence-based practice in allied health care such as a lack of time,
skills and resources. 10 Targeted approaches need to be used
to support allied health clinicians to change their practice in response
to emerging evidence. 11
Methods of professional learning have traditionally included
conferences, workshops, courses and journal clubs delivered in face to
face settings. Online learning platforms are systems that enable
learners to access educational content digitally, typically through the
use of websites or mobile phone applications. The use of online
learning platforms to assist knowledge translation is emerging, with a
rapid increase in online learning adopted during the COVID-19 pandemic
when traditional face-to-face learning opportunities were limited.
12, 13 Online learning platforms can facilitate synchronous or
asynchronous delivery of information, or a combination of these two
modes of learning. They can teach knowledge or skills through
structured online courses, provide access to information through apps
or databases with built in decision aids or connect people through
online communities of practice. 14-16 Online learning
platforms may be used alone, or in combination with other modes of
education delivery. 17
Online learning platforms have been widely reported in the literature
and can enable access to learning opportunities that may otherwise be
limited by geographical barriers, time or resources. 10, 18
The use of online learning platforms has potential to facilitate the
translation of knowledge into clinical practice across a range of
clinical settings, by enhancing access to knowledge translation
interventions. However, it is also possible that online learning
platforms lack known strategies required to change behaviour, such as
practical skill acquisition, identification of champions, and adaptation
of knowledge translation to the local environment. 19, 20
Several systematic reviews have synthesised literature in fields
related to e-learning and the allied health professions. Rohwer et al.
20 evaluated the use of e-learning on increasing
competencies in healthcare professions including medical, nursing and
allied health and found that e-learning increased competencies
(comprised of knowledge and skills) although not behaviour or
attitudes. A systematic review of 16 randomised controlled trials by
Vaona et al. (2018), found that e-learning was comparable to
face-to-face learning in improving patient outcomes or knowledge, skill
or behaviour of health professionals. 21 Dizon et al.
reviewed studies (n=6) investigating evidence-based practice training
across all modalities (including face-to-face training) for allied
health professionals and highlighted that there is limited research but
some evidence that training improves knowledge, skills and attitudes in
this population. 22 However, questions remain over the role
of online learning platforms for knowledge translation in the allied
health professions, and whether they are effective in bringing about
changes to clinical practice.
The aims of this systematic review were to synthesise current evidence
on: (1) the effectiveness of online learning platforms for improving
the knowledge, skills, and confidence of allied health professionals;
and (2) the impact of knowledge translation interventions delivered
electronically on clinical practice in the allied health professions.
Methods
Protocol and registration
Methods for this review were developed in advance and registered with
PROSPERO (registration number CRD42020147013). The review is reported
in accordance with the PRISMA 2020 guidelines. 23
Search Strategy
A comprehensive electronic search of original research literature was
conducted in Medline-Ovid, CINAHL and Embase from the earliest
available date to November 2023. Search terms and keywords that were
used to complete the search included the three domains of: (1) online
delivery (and synonyms such as technology, e-learning, and electronic);
(2) learning (and synonyms such as teaching, training and education);
and (3) knowledge translation (and synonyms such as evidence uptake,
implementation, diffusion of innovation). MeSH headings were utilised
in addition to keyword searches. Synonyms within the three domains were
combined with the OR operator, then results combined using the AND
operator. The researchers reviewed the reference lists and citations of
included papers to identify further papers that met the inclusion
criteria but were not identified in the initial database search.
Selection Criteria
Inclusion criteria encompassed: (a) peer-reviewed papers in which
allied health professionals (minimum 50% of the sample)
participated in online learning for the purpose of translating
knowledge into practice; (b) the majority of the learning component
(at least 60%) was delivered electronically (such as through videos,
access to online resources, mobile phone apps or chat rooms); (c)
comparative data were reported (either pre post or between group
comparisons) on any quantitative outcome of a knowledge translation
initiative. Allied health therapy professions included in this
review were occupational therapy, speech pathology, social work,
dietetics, physiotherapy and podiatry, aligning with
classifications by Turnbull et al.
8 Only studies published in English were included due to
lack of resources for translation. Papers were excluded if they were
book chapters, conference abstracts, theses, or review papers.
Selection Process
The title and abstract of all papers retrieved in the initial search
were downloaded into the online platform Covidence 24 and
screened independently by two reviewers who applied the inclusion and
exclusion criteria. The reviewers discussed any disagreement until a
consensus was reached for papers to progress to review of the full text
papers, with provision to call upon a third reviewer if required. Full
text papers were retrieved for all studies that remained after the
title and abstract screening, with the same process applied. The
reference lists were checked and citations tracked of all included
papers to check for any additional studies that may have been missed in
the initial search.
Quality appraisal
Quality appraisal was conducted by two independent reviewers using the
Downs and Black Checklist25. This 27-item appraisal tool was
designed for use with both randomised controlled trials and
non-controlled trials. As a guide to interpretation, quality of studies
can be considered excellent (score 26-32), good (20-25), fair (15-19)
or poor (14). 26 Consensus was achieved through discussion
between two reviewers. Scoring for the final question relating to
whether the study had sufficient power to observe a clinically important
difference25was conducted using methods described
by Speed and Harding27. Studies were allocated a score of 5,
3 or 0 based on good evidence of adequate power, marginal evidence of
adequate power or lack of any evidence of adequate power respectively.
Studies were not excluded from the review based on the quality
appraisal, but study quality was considered in the interpretation of
findings.
Data Extraction and Synthesis
Data were extracted using a custom-designed data extraction form. The
data were extracted from each included study by one reviewer, with the
results checked by a second member of the review team. The results were
organised into tables by the type of outcome measured for descriptive
synthesis. Meta-analyses were undertaken for studies with appropriate
levels of homogeneity, using Review Manager 5.4.1 software 28
with a random effects model. Standard mean differences were used to
allow comparison of studies measuring knowledge change on different
scales. Studies with pre-post designs as well as controlled studies
were considered for inclusion in meta-analyses; while this approach has
limitations, meta-analyses of pre-post effect sizes can be of value,
particularly in fields where randomised controlled trials are rarely
conducted. 29 The I2statistic was used as an
indication of heterogeneity30.
Results
Yield
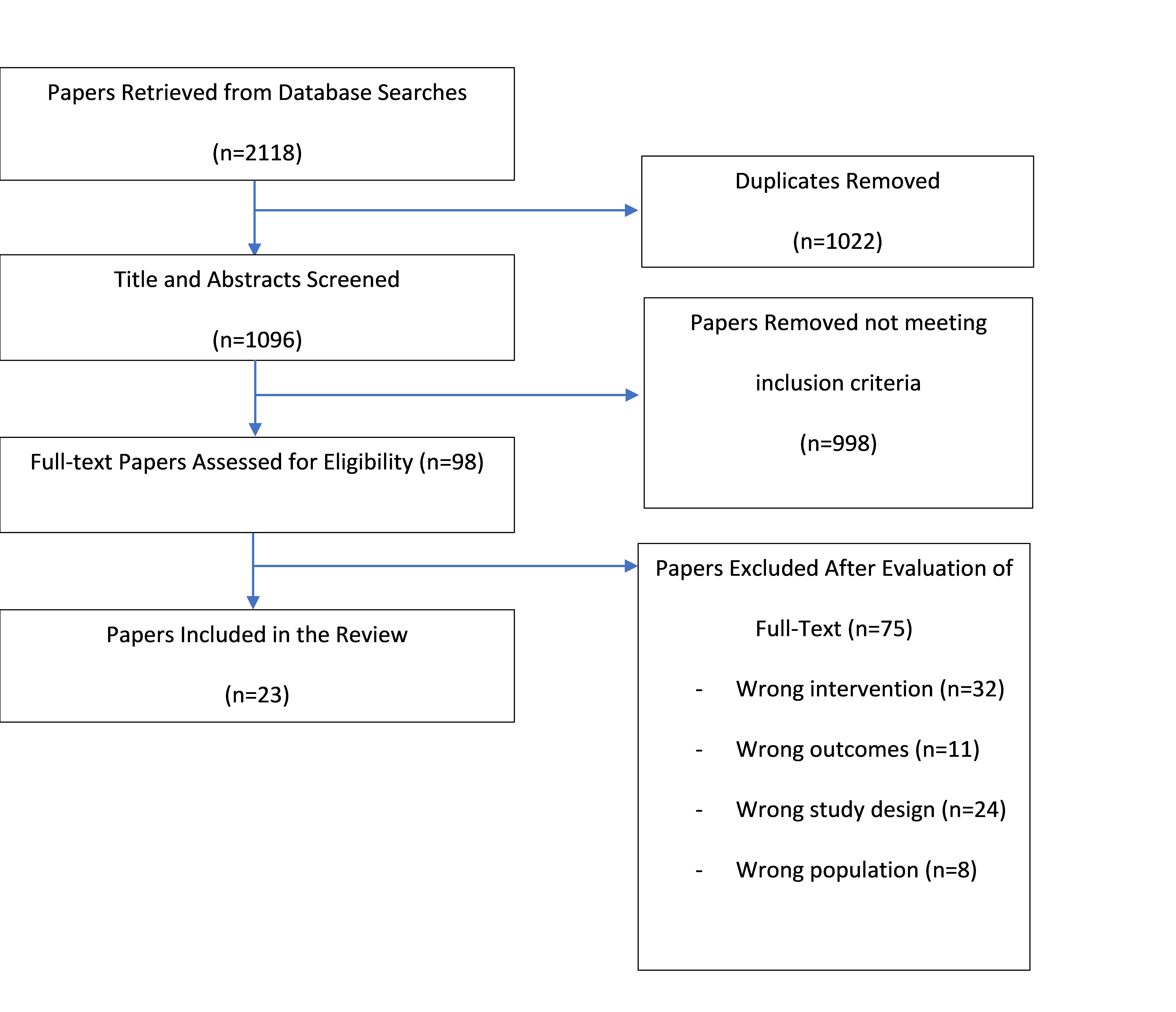
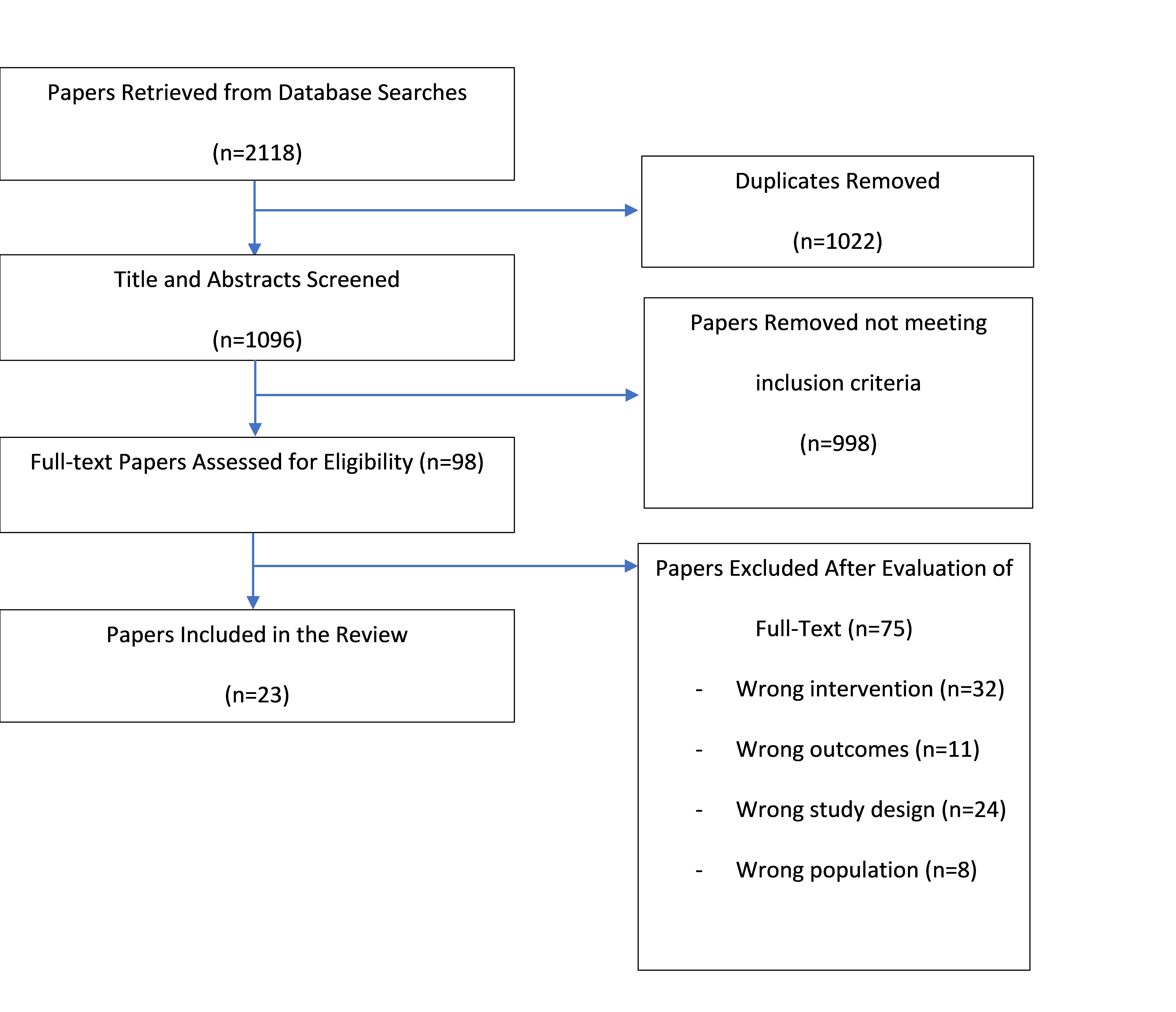
A total of 2118 papers resulted from the literature search, of which
1022 duplicates were removed. One additional paper was located through
reference list checking or citation tracking. A total of 998 papers
were excluded based on title and abstract. There was over 90% agreement
between reviewers on title and abstract screening; for those with
discrepancies (n=106), agreement was reached by consensus without the
need for a third reviewer. Evaluation of full text was undertaken for
98 papers. A further 75 papers were excluded because: they did not
evaluate an intervention that met the definition of online delivery
(n=32); comparative outcomes of quantitative data were not reported
(n=35); or the paper did not focus on allied health professionals (n=8)
(Figure 1). The final library of included studies contained 23 papers.
14, 31-50
Figure 1. Flow of studies through the review. Papers may have been
excluded for failing to meet more than one inclusion criteria
Summary of included papers
Of the 23 papers included in the review, ten studies were based in
Canada, 14, 32, 34, 35, 40-43, 49, 50 four in the United
States of America, 33, 36, 39, 45 two in Australia,
37, 46
and one each in Mexico 51 and South Korea. 38 One
study included participants from Israel, Canada and Australia.
44
The four remaining studies were open to participants from any country
without specified geographical boundaries. 31, 47, 48, 52
Most studies (n=18) focused on online learning only with the remaining
five studies employing blended learning with the inclusion of a
minority face-to-face training component. All studies included at least
one online learning module or webinar as a part of their training
program. Seventeen studies used pre-post designs, three were clinical
trials, one used a case study design, one used mixed methods (website
analytics and quantitative survey) and one used a cross-sectional
survey design. The knowledge to be translated was very diverse; for
example, topics of study included tracheostomy care, electrical
stimulation, determining decision making capacity and returning to
driving following stroke37, 43, 44, 48. All reported measures
of knowledge acquisition (including knowledge, skill, or confidence),
six studies reported measures of attitude including intent to change
practice, and seven studies measured practice change. A summary of
the included papers is presented in Table 1.
Quality appraisal
The quality of the included papers was appraised by two reviewers using
the Downs and Black 25 checklist (Table 1), with all
disagreements resolved by consensus without the need for a third
reviewer. The Downs and Black scores ranged from seven to 29 (Table 1).
The most common criteria that were not addressed in the included
studies were randomisation of the intervention, blinding of study
subjects to the intervention, and clear reporting of the main outcomes
of the studies.
Table 1. Summary of included studies
|
Study ID
|
QA*
|
Setting
|
Participants
|
Knowledge for translation
|
Study design
|
Intervention**
|
|
Applebaum 31
|
19
|
Oncology care, worldwide
|
Healthcare professionals and students (n=46)
|
Acute cancer cognitive therapy
|
Pre post. Baseline, post training.
|
Online: 5x modules including teaching content, case
scenarios, quizzes (AS)
|
|
Atack 32
|
19
|
Hospital settings in Canada
|
Healthcare professionals (n=76)
|
Infection control and prevention
|
Pre post. Baseline, 2x post within 2 weeks of
learning.
|
Online: 3 modules including video, quizzes, games
(AS)
|
|
Beissner 33
|
22
|
Visiting nurse service in New York, USA
|
Physiotherapists (n=238)
|
Pain self-management program
|
Cluster randomised controlled trial.
|
Blended: Online manual, videos, sample scripts (AS);
2x half day face to face sessions (S).
|
|
Camden 34
|
17
|
Paediatric care in Canada
|
Physiotherapists (n=50)
|
Developmental Coordination Disorder
|
Pre post. Baseline; post training; 2 months post.
|
Online: 5x learning modules (AS)
|
|
Chepeha 35
|
18
|
Post-surgical shoulder care in Alberta, Canada
|
Physiotherapists (n=181)
|
Postoperative shoulder pain
|
Mixed methods. Website analytics, quantitative
survey.
|
Online: Guideline including narrated presentations
and video demonstrations (AS)
|
|
Cunning-ham 14
|
20
|
Paediatrics services, Ontario, Canada
|
Speech pathologists (n=52)
|
Communication function classification system
|
Pre post. Baseline, post completion of training.
|
Online: PowerPoint presentation, case scenarios,
literature (AS)
|
|
Drabkin 36
|
24
|
Public, community health services USA
|
Intimate partner violence (IPV) workers (n=156)
|
IPV Prevention
|
Pre post. Baseline; 3 months post.
|
Online only: 13 interactive modules using video, fact
sheets and exercises (AS)
|
|
Frith 37
|
14
|
Stroke care in Australia
|
Health professionals (n=12)
|
Return to driving guidelines
|
Pre post. Baseline; post training
|
Online: 30-minute e-learning module (AS)
|
|
Heitman 51
|
17
|
Nutrition care in Mexico
|
Nutrition and dietetics professionals (n=11)
|
Nutrition care process
|
Pre post. Baseline; post training.
|
Online: Prework 4 hrs (AS), web-based training (S),
post training support
|
|
Jeong 38
|
15
|
Paediatric care in South Korea
|
Occupational therapists and educators (n=27)
|
Measuring participation of children with disabilities
|
Cross-sectional survey post training.
|
Online: 23-minute webinar including PowerPoint
presentation (AS)
|
|
Jorge 52
|
18
|
Osteoarthritis care, worldwide
|
Physiotherapists, dietitians, podiatrists (n=784)
|
Knee osteoarthritis care via telehealth
|
Pre post. Baseline; post training; 4 months post.
|
Online: E-learning modules (3-4hrs), videos, resources
|
|
Kobak 39
|
22
|
Paediatric mental health services, USA
|
Licensed clinicians (n=18)
|
Integrating technology into CBT for depression
|
Pre post. Baseline, post training.
|
Online: 5.5-hour interactive modules including video
(AS)
|
|
Levac 40
|
17
|
Stroke rehabilitation in Canada
|
Physiotherapists and occupational therapists (n=11)
|
Motor learning and virtual reality stroke
rehabilitation
|
Pre post. Post initial training and post
implementation
|
Blended: 3x online modules, reminder email, practice
(AS), 3x face-to-face sessions (S)
|
|
Lingum 41
|
20
|
Long-term care homes in Canada
|
Healthcare professionals (n=133)
|
Caring for frail, medically complex older adults
|
Pre post. Baseline; post sessions; program completion
|
Online only: Weekly 1-hour online learning sessions
over 12 weeks (S)
|
|
Miller 42
|
18
|
Pediatric cerebral palsy care in Canada
|
Pediatric physical and occupational therapists
(n=102)
|
Hip surveillance in cerebral palsy
|
Pre post. Baseline; 1 year follow up.
|
Blended learning: Webinars (S), learning module,
presentations, clinician booklet (AS)
|
|
Orr 43
|
22
|
Home care providers in Canada.
|
Healthcare professionals (n=83)
|
Electrical stimulation
|
Pre post. Baseline, post training, post workshop.
|
Blended: 8x online training modules (AS) and 1x
face-to-face workshop (S).
|
|
Pesiah 44
|
17
|
Aged care in Israel, Canada, and Australia.
|
Healthcare professionals (n=31)
|
Determining decision making capacity
|
Pre post. Baseline; post training.
|
Online: 25-minute module adapted based on pre-test
results (AS)
|
|
Robitaille 49
|
18
|
Canadian armed forces
|
Physiotherapists (n=67)
|
Ankle sprain management
|
Pre post. Baseline; post training.
|
Blended: Recorded presentation delivered synchronously
with peer discussion.
|
|
Roberts 45
|
7
|
USA
|
Dietitians (n=2)
|
Nutrition practice guidelines
|
Case study design
|
Online: webinar training session (S)
|
|
Sarkies 46
|
29
|
Public health services in Melbourne, Australia
|
Nursing and allied health clinicians. (n=119)
|
Physical activity after DVT, Falls prevention
strategies
|
Randomised Controlled Trial
1x survey
|
Online: Video summaries compared with written summaries
(AS)
|
|
Scrivener 47
|
10
|
Australian university (learners worldwide)
|
Student and qualified physiotherapists (n=174)
|
Task specific training
|
Pre post. Baseline; post training.
|
Online: 5x modules including video demonstrations (AS)
|
|
Szekeres 50
|
19
|
Rehabilitation in Canada
|
Physiotherapist (n=98) and occupational therapists
(n=26)
|
Rehabilitation outcomes measures
|
Trial comparing online with face to face training.
|
Online: 8-10 hours learning content and independent
learning (AS); discussion with facilitator (S)
|
|
Swords 48
|
18
|
22 countries globally
|
Health professionals, patients/caregivers (n=103)
|
Tracheostomy care
|
Pre post. Baseline assessment, post-webinar
assessment.
|
Online: 5x webinar sessions, professional discourse
over 12 months (S)
|
*QA: Quality appraisal Score out of 27 on the Downs and Black Checklist
24
**Synchronous and asynchronous indicated by (S) or (AS)
Knowledge-Related Outcomes
Across the included studies, knowledge-related outcomes were described
in the domains of knowledge acquisition, skill acquisition and
confidence. All included studies reported on at least one measure in the
knowledge category. Nineteen of the 23 studies evaluated knowledge
acquisition, four studies evaluated skill acquisition and seven studies
evaluated the self-reported confidence of participants in their ability
to apply knowledge following the intervention. Table 2 summarises the
key findings from all included studies. One study could be described as
excellent, 46 six as good, 14, 33, 36, 39, 41, 43
thirteen as fair 31, 32, 34, 35, 38, 40, 42, 44, 48-52 and
three as poor 37, 45, 47 based on the Downs and Black score.
26
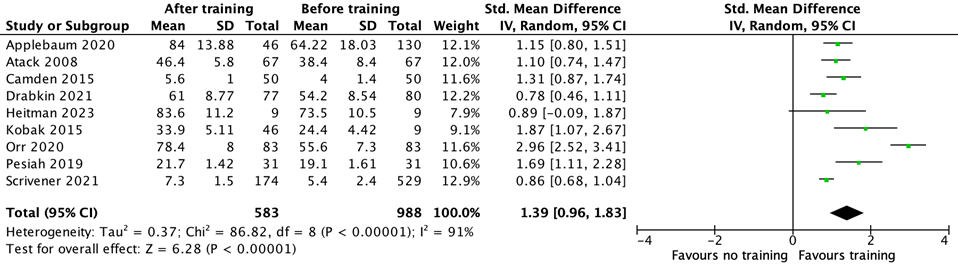
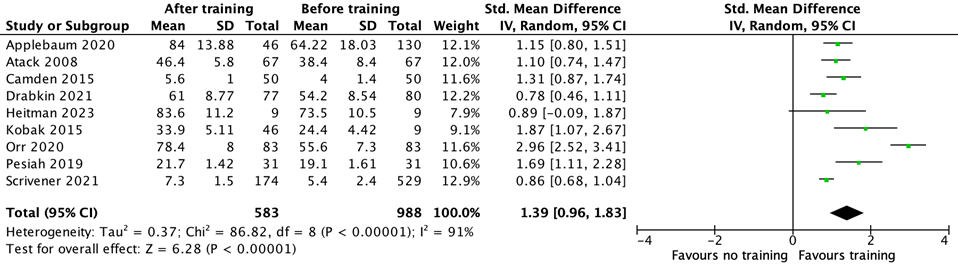
There was sufficient data presented in n=9 studies to be combined in a
meta-analysis, which showed a significant improvement in knowledge
after the online learning (standard mean difference 1.39; 95% CI =
0.96, 1.83; p-value <0.01; I²=91%),
31, 32, 34, 36, 39, 43, 44, 47, 51
although the high I 2 value suggests heterogeneity in the
analysis (Figure 2). All but one study included in the meta-analysis
were rated fair or good quality studies.
For those studies who reported on knowledge acquisition but were not
included in the meta-analysis (n=10), all reported improved knowledge
associated with the intervention.
14, 35, 37, 38, 42, 45, 46, 48-50
Three fair or good quality studies demonstrated this improvement to be
statistically significant. 14, 42, 48 The remaining seven
studies, with quality ranging from poor to excellent, reported
descriptive observations only. 35, 37, 38, 45, 46, 49, 50
One study showed a statistically significant improvement with knowledge
acquired through video summaries, compared with no improvement through
written summaries. 46
Of four studies measuring skill acquisition two reported a
statistically significant improvement. 14, 32 One study
reported descriptive observations. 49 One fair quality study
did not find any significant difference in clinical reasoning skills
following online training. 40
An increase in confidence following online learning was measured in
seven studies. 31, 33, 36, 40, 41, 48, 52 Confidence improved
in all seven studies, with four studies of fair or good quality
demonstrating statistical significance of their results.
36, 40, 41, 48
Figure 2. Meta-analysis of knowledge acquisition
Attitudes
Outcomes related to attitudes towards knowledge or skill acquired
through online learning platforms were reported in n=6 studies.
14, 32, 41, 43, 50, 52
Three studies measured receptivity towards behaviour change based on
the content learned through online learning platforms.
32, 43, 50
Three studies reported intent for future use of the knowledge or skill
acquired through the online learning platform. 14, 41, 52
These six studies, of fair or good quality, reported that participants
were receptive to change, or most participants had an intention to
change their future clinical practice following engagement with an
online learning platform.
Behaviour Change
Outcomes related to behaviour change, (for example, actual change to
clinical practice), were measured in n=7 studies.
33, 36, 39, 40, 45, 51, 52
Two studies provided evidence of self-reported improvements in
implementation of guidelines following online learning interventions,
one relating implementation of a nutrition clinical guideline
45
and the other in the field of knee osteoarthritis. 52 One
study reported a statistically significant improvement in the delivery
of only one out of six areas of pain self-management training delivered
by an allied health professional. 33 The remaining four
studies reported no difference in practice following engagement with an
online learning platform designed to change practice in the fields of:
intimate partner violence prevention; integrating technology into
cognitive behavioural therapy for depression; using motor learning
strategies within virtual reality stroke rehabilitation; and a virtual
nutrition care process. 36, 39, 40, 51
Table 2. Summary of key knowledge, attitude and behaviour change
outcomes
|
Education Focus
|
Education Components
|
Paper
|
Direction of Change
|
|
Knowledge gain
|
Knowledge
|
Applebaum 31
|
Improved knowledge in acute cancer cognitive therapy
(p<0.01)
|
|
Atack 32
|
Improved knowledge in infection prevention and
control (p<0.01)
|
|
Camden 34
|
Improved knowledge of developmental coordination
disorder (p<0.05)
|
|
Chepeha 35
|
Improved knowledge in postoperative shoulder care
|
|
Cunningham 14
|
Improved knowledge in methods for using the
Communication Function Classification System (CFCS)
(p<0.01)
|
|
Drabkin 36
|
Improved knowledge of intimate partner violence
prevention-related topics (p<0.01)
|
|
Frith 37
|
Improved knowledge of Australian return to driving
guidelines
|
|
Heitman 51
|
Improved knowledge of Nutrition Care Process
(p<0.01)
|
|
Jeong 38
|
Improved knowledge of participation in children with
disabilities
|
|
Kobak 39
|
Improved knowledge of CBT concepts (p<0.01)
|
|
Miller 42
|
Improved knowledge in hip surveillance for children
with cerebral palsy in 15/16 knowledge areas. 5/16
areas (p<0.05)
|
|
Orr 43
|
Improved knowledge of electrical stimulation
(p<0.01)
|
|
Pesiah 44
|
Improved knowledge in determining decision making
capacity (p<0.01)
|
|
Robitaille 49
|
Improved knowledge of comprehensive rehabilitation
program
|
|
Roberts 45
|
Improved knowledge of critical illness
recommendations, used to create protocol reported by 60%
of respondents (n=6)
|
|
Sarkies 46
|
Improved knowledge with video summaries (p<0.01),
but not written summaries
|
|
Scrivener 47
|
Improved knowledge in task specific training.
Standard mean difference 0.85
|
|
Szekeres 50
|
Improved knowledge in rehabilitation outcome measures
from 51.1% to 55.4%
|
|
Swords 48
|
Improved knowledge in decannulation (p<0.01)
|
|
Skills
|
Atack 32
|
Improved competence in infection prevention and
control (p<0.01)
|
|
Cunningham 14
|
Improved skill in classifying a child using the CFCS
(p<0.01)
|
|
Levac 40
|
No significant change in clinical reasoning skills
related to motor learning strategies
|
|
|
Robitaille 49
|
Improved performance in comprehensive rehabilitation
program
|
|
Confidence
|
Applebaum 31
|
Improved confidence working in cancer care reported
by 75% of respondents (n=38)
|
|
Beissner 33
|
80% respondents reported confidence in teaching the
pain self-management program
|
|
Drabkin 36
|
Improved self-efficacy scores in intimate partner
violence prevention strategies (p<0.01)
|
|
Jorge 52
|
Improved confidence with videoconferencing. Mean
change 3.1/10 (95% CI 3.0-3.3)
|
|
Levac 40
|
Improved confidence in motor learning strategies in
virtual reality rehabilitation (p<0.01)
|
|
Lingum 41
|
Improved confidence in working with residents with
COVID-19 (p<0.01)
|
|
Swords 48
|
Improved confidence in decannulating children
(p<0.05)
|
|
Attitude
|
Attitude
|
Atack 32
|
Majority of respondents keen to adopt change.
|
|
Orr 43
|
Improved attitude towards electrical stimulation to
stimulate healing p<0.05.
|
|
Szekeres 50
|
Significant increase in readiness for change
following online learning; no difference compared
with face to face group.
|
|
Intent for
future use
|
Cunningham 14
|
Intention for future use of CFCS from 81% (n=42) of
respondents
|
|
Jorge 52
|
Improved likelihood to use education. Mean change
0.4/10 (95% CI 0.3-0.5)
|
|
Lingum 41
|
Intention to change behaviour by 63% of respondents
|
|
Behaviour Change
|
Practice change
|
Beissner 33
|
Significant improvement in documentation of the use
of imagery (p<0.01), but no difference in
documentation of other six domains measured.
|
|
Drabkin 36
|
No statistically significant difference in
utilisation of intimate partner violence strategies
following online learning
|
|
Heitman 51
|
Quality of clinical notes using a validated audit
tool showed low quality clinical notes and no
resolution of nutrition problems.
|
|
Jorge 52
|
Self-reported implementation e-learning knowledge
reported by 99.3% of participants.
|
|
Kobak 39
|
No statistically significant difference in clinical
ratings of improvement for CBT group.
|
|
Levac 40
|
No significant practice change with motor learning
strategies (p=0.092)
|
|
Roberts 45
|
Improved implementation of critical illness guideline
reported by 70% of respondents (n=7)
|
DISCUSSION
All studies in this review found that the knowledge, skill, or
confidence of allied health professionals improved through engagement
with online learning platforms. This finding was consistent with
previous studies evaluating outcomes of online learning involving
allied health, nursing and medical professionals.
17 However, few of the included studies measured change in
clinical practice, and the findings of those that did also concurred with
previous studies suggesting that online learning alone is not sufficient to
change behaviour. 17, 20 Most of the studies included in this
review were observational designs with a high risk of bias and overall
confidence in the findings is low, but the findings highlight current gaps
in understanding of the potential role of online learning platforms for
supporting the translation of knowledge into practice.
Online learning platforms offer many benefits in the dissemination of
information that are likely to contribute to the success of these programs
in the acquisition of knowledge. For example, online learning provides
opportunities for multimodal delivery of content, using video, audio,
written materials, interactive activities, links to wider resources and
connections with others. Consistent with principles of adult learning,
online platforms also have the potential to tailor information based on
users' experience or prior knowledge and enable self-paced and autonomous
learning. 53 There are also many situations in which online
learning platforms may offer advantages over face-to-face training by
reducing travel time, overcoming geographical boundaries, or providing
flexibility to complete training asynchronously at a time that is
preferable for the learner. Online learning provides a potentially low cost
and accessible way to disseminate information and may therefore be ideally
suited to situations where the desired outcome is an improvement in
knowledge, skill, or confidence.
However, it is not enough for allied health clinicians to complete online
training and expect a change in clinical practice. This phenomenon is not
unique to online learning platforms, with a systematic review by Scott et
al. 11 highlighting multiple studies reporting that education
alone has minimal influence on changing clinical practice. These findings
align with current implementation science literature suggesting a need for
a broader approach to knowledge translation 19, 54 The COM-B
framework for behaviour change acknowledges that capacity (encompassing but
not limited to knowledge and skills) is a necessary component, but also
stresses the importance of opportunity and motivation as factors
contributing to behaviour change success. 55 Examples of more
active approaches to translating knowledge into practice in the allied
health professions have included the use of knowledge brokers, electronic
evidence libraries and clinical outcomes databases, and tailoring
strategies to address barriers to change. 7, 56
The findings of this review have implications for policy makers, clinical
educators, and clinicians. Policy makers and clinical educators should
acknowledge the potential role for online learning as an accessible and low
cost alternative to face to face learning for increasing clinicians'
knowledge, skill, or confidence. However, these same policy makers and
clinical educators need to be aware of the need to employ time and
resources to facilitate the translation of the acquired knowledge into
clinical practice above and beyond providing funding support or professional
development leave. This concept has been explored by Hitch and colleagues
57 who defined four key stages of intervention required to
support knowledge translation being: doing knowledge translation
(knowledge, timeframes, align with theory, resources), social capital for
knowledge translation (leadership, social networks, social skill sets),
sustaining knowledge translation (discipline focus, capacity building,
linked to organisational strategy, evaluating outcomes of knowledge
translation), and inclusive knowledge translation (broaden beyond the team,
dissemination strategies). Addressing these factors in the context of online
learning may be challenging but potential solutions are emerging. Levac and
colleagues, 58 for example, have proposed best practice
recommendations for the development of online knowledge translation
resources. Future studies could consider integrating a learning module into
a training package that focuses on known knowledge translation strategies
and frameworks, as a complement to the clinical knowledge content.
Providing information about the need for deliberate, tailored attention to
implementation strategies alongside learning modules designed to increase
clinical knowledge and skills and confidence may be one potential mechanism
for increasing the likelihood that knowledge acquired through online
learning will be embedded into clinical practice.
This review was limited to studies published in the English language only
which may have impacted on the inclusion of some international studies that
could inform this review. There are a wide range of terms that are used to
describe both knowledge translation and education which may have impacted
on the search design. However, only one additional paper was found through
citation checking so it is likely that our search has been successful in
finding the available relevant literature. The meta-analysis in this review
needs to be interpreted with caution, given that most of the studies used
pre-post designs and many were of low quality with a high risk of bias.
However, inclusion of this analysis provides a useful overview of current
evidence in this field.
CONCLUSION
Online learning is an effective way of improving clinicians' knowledge,
skill and/or confidence and attitude towards future use of the learned
content. Online learning alone does not necessarily lead to a change in
clinical practice. Known strategies that support the gap between knowledge
and clinical practice should be employed to ensure that clients reap the
benefits of investment into ongoing learning of clinicians. Policy makers
and clinical educators can play a key role in prioritising the accompanying
knowledge translation strategies required to facilitate practice change.
REFERENCES
1. Graham ID, Straus SE, Tetroe J, ProQuest. Knowledge
translation in health care moving from evidence to practice. 2nd ed.
Chichester, West Sussex: John Wiley & Sons; 2013.
2. Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An
introduction to implementation science for the non-specialist. BMC
Psychology. 2015;3(1):32.
3. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is
the question: understanding time lags in translational research. Journal of
the Royal Society of Medicine. 2011;104(12):510-20.
4. Braithwaite J, Glasziou P, Westbrook J. The three numbers you
need to know about healthcare: the 60-30-10 Challenge. BMC Medicine.
2020;18(1):102.
5. Khalil H. Knowledge translation and implementation science:
what is the difference? JBI Evidence Implementation. 2016;14(2).
6. Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell
W, Robinson N. Lost in knowledge translation: Time for a map? The Journal
of Continuing Education in the Health Professions. 2006;26(1):13-24.
7. Cahill LS, Carey LM, Lannin NA, Turville M, Neilson CL, Lynch
EA, McKinstry CE, Han JX, O'Connor D. Implementation interventions to
promote the uptake of evidence-based practices in stroke rehabilitation.
Cochrane Database of Systematic Reviews. 2020;10(10):CD012575.
8. Turnbull C, Grimmer-Somers K, Kumar S, May E, Law D, Ashworth
E. Allied, Scientific and Complementary Health Professionals: A New Model
for Australian Allied Health. Australian Health Review. 2009;33(1):27-37.
9. Barrimore SE, Cameron AE, Young, AM, Hickman, IJ, Campbell, KL.
Translating Research Into Practice: How Confident Are Allied Health
Clinicians? Journal of Allied Health. 2020;49(4):258-62.
10. Harding KE, Porter J, Horne‐Thompson A, Donley E, Taylor NF. Not
Enough Time or a Low Priority? Barriers to Evidence‐Based Practice for
Allied Health Clinicians. The Journal of Continuing Education in the Health
Professions. 2014;34(4):224-31.
11. Scott SD, Albrecht L, O'Leary K, Ball GDC, Hartling L, Hofmeyer
A, Jones A, Klassen TP, Burns, KK, Newton AS, Thompson D, Drydon, D.
Systematic review of knowledge translation strategies in the allied health
professions. Implementation Science. 2012;7(1):70.
12. Khurshid Z, De Brún A, Moore G, McAuliffe E. Virtual adaptation
of traditional healthcare quality improvement training in response to
COVID-19: a rapid narrative review. Human Resources for Health.
2020;18(1):81.
13. Malik M, Valiyaveettil D, Joseph D. Optimizing e-learning in
oncology during the COVID-19 pandemic and beyond. Radiation Oncology
Journal. 2021;39(1):1-7.
14. Cunningham BJ, Rosenbaum P, Hidecker MJC. Promoting consistent
use of the communication function classification system (CFCS). Disability
and Rehabilitation. 2016;38(2):195-204.
15. Hancock NJ, Collins K, Dorer C, Wolf SL, Bayley M, Pomeroy VM.
Evidence-based practice 'on-the-go': using ViaTherapy as a tool to enhance
clinical decision making in upper limb rehabilitation after stroke, a
quality improvement initiative. BMJ Open Quality. 2019;8(3):e000592.
16. Pyrko I, Dörfler V, Eden C. Thinking together: What makes
Communities of Practice work? Human Relations (New York).
2017;70(4):389-409.
17. Rohwer A, Motaze NV, Rehfuess E, Young T. E‐learning of
evidence‐based health care (EBHC) to increase EBHC competencies in
healthcare professionals: a systematic review. Campbell Systematic Review.
2017;13(1):1-147.
18. Vera M, Kattan E, Cerda T, Niklitshek J, Montaña R, Varas J,
Corvetto M. Implementation of Distance-Based Simulation Training Programs
for Healthcare Professionals: Breaking Barriers During COVID-19 Pandemic.
Simulation in Healthcare : Journal of the Society for Medical Simulation.
2021;16(6):401-6.
19. Michie S. Designing and implementing behaviour change
interventions to improve population health. Journal of Health Services
Research & Policy. 2008;13:64-9.
20. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery
JC. Fostering implementation of health services research findings into
practice: a consolidated framework for advancing implementation science.
Implementation Science. 2009;4(1):50.
21. Vaona A, Banzi R, Kwag KH, Rigon, G, Cereda D, Pecoraro V,
Tramacere I, Moja, L. E-learning for health professionals. Cochrane
database of systematic reviews. 2018(1):CD011736.
22. Dizon JMR, Grimmer-Somers KA, Kumar S. Current evidence on
evidence-based practice training in allied health: a systematic review of
the literature. International Journal of Evidence-based Healthcare.
2012;10(4):347-60.
23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow
CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J,
Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E,
McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA,
Whiting P, Moher, D. The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. International Journal of Surgery.
2021;88:105906.
24. Covidence systematic review software, Veritas Health Innovation,
Melbourn, Australia. Available at
www.covidence.org
25. Downs SH, Black N. The feasibility of creating a checklist for the
assessment of the methodological quality both of randomised and
non-randomised studies of health care interventions. Journal of
Epidemiology and Community Health. 1998;52(6):377-84.
26. Hooper P, Jutai JWP Strong G, Russell-Minda E. Age-related macular
degeneration and low-vision rehabilitation: a systematic review. Canadian
journal of ophthalmology. 2008;43(2):180-7.
27. Speed LB, Harding KE. Tracheostomy teams reduce total tracheostomy
time and increase speaking valve use: A systematic review and
meta-analysis. Journal of Critical Care. 2013;28(2):216.e1-.e10.
28. Review Manager Web (RevMan Web). The Cochrane Collaboration; 2020.
29. Kösters M. Every effect size has its place: a commentary on the
avoidance of pre-post effect sizes. Epidemiology and psychiatric sciences.
2017;26(4):369-70.
30. Melsen WG, Bootsma MCJ, Rovers MM, Bonten MJM. The effects of
clinical and statistical heterogeneity on the predictive values of results
from meta-analyses. Clinical microbiology and infection. 2014;20(2):123-9.
31. Applebaum A, Walsh LE, Polacek LC, Benvengo S, Levin T. Acute
Cancer Cognitive Therapy Online Training Program: Feasibility and Impact on
Clinician Knowledge Uptake. Journal of Cancer Education. 2021;36(5):1081-5.
32. Atack L, Luke R. Impact of an online course on infection control
and prevention competencies. Journal of Advanced Nursing.
2008;63(2):175-80.
33. Beissner KL, Bach E, Murtaugh CM, Trifilio M, Henderson JCR,
Barrón Y, Trachtenberg MA, Carrington Reid M. Translating Evidence-Based
Protocols Into the Home Healthcare Setting. Home Healthcare Now.
2017;35(2):105-12.
34. Camden C, Rivard L, Pollock N, Missiuna C. Knowledge to Practice
in Developmental Coordination Disorder: Impact of an Evidence-Based Online
Module on Physical Therapists' Self-Reported Knowledge, Skills, and
Practice. Physical & Occupational Therapy in Pediatrics.
2015;35(2):195-210.
35. Chepeha JC, Silveira A, Sheps D, Beaupre LA, Shoulder and Upper
Extremity Research Group of Edmonton (SURGE). Evaluating the Uptake and
Acceptability of Standardized Postoperative Rehabilitation Guidelines Using
an Online Knowledge Translation Approach. Physical Therapy.
2020;100(2):225-37.
36. Drabkin AS, Baden L, Solomon J, Card JJ. IMPACT: Effects of an
Online Capacity-Building Intervention for IPV Prevention Professionals.
Journal of Interpersonal Violence. 2021;36(15-16):NP7899-NP919.
37. Frith J, Hubbard I, James C, Warren-Forward H. In the Driver's
Seat: Development and Implementation of an e-Learning Module on
Return-to-Driving After Stroke. Occupational Therapy in Health Care.
2017;31(2):150-61.
38. Jeong Y, Law M, DeMatteo C, Stratford P, Kim H. Knowledge
Translation from Research to Clinical Practice: Measuring Participation of
Children with Disabilities. Occupational Therapy in Health Care.
2016;30(4):323-43.
39. Kobak KA, Mundt JC, Kennard B. Integrating technology into
cognitive behavior therapy for adolescent depression: a pilot study. Annals
of General Psychiatry. 2015;14(37):37.
40. Levac DE, Glegg SMN, Sveistrup H, Colquhoun H, Miller P, Finestone
H, DePaul V, Harris JE, Velikonja D. Promoting Therapists' Use of Motor
Learning Strategies within Virtual Reality-Based Stroke Rehabilitation.
PloS One. 2016;11(12):e0168311.
41. Lingum NR, Sokoloff LG, Meyer RM, Gingrich S, Sodums DJ, Santiago
AT, Feldman S, Guy S, Moser A, Shaikh S, Grief CJ, Conn DK. Building
Long-Term Care Staff Capacity During COVID-19 Through Just-in-Time
Learning: Evaluation of a Modified ECHO Model. Journal of the American
Medical Directors Association. 2021;22(2):238-44.
42. Miller S, O'Donnell M, Mulpuri K. Physical Therapists Are Key to
Hip Surveillance for Children with Cerebral Palsy: Evaluating the
Effectiveness of Knowledge Translation to Support Program Implementation.
Physical & Occupational Therapy in Pediatrics. 2021;41(3):300-13.
43. Orr L, Houghton P, Holyoke P, Lala D. A Quasi-Experimental
Evaluation of an Education Program for the Use of Electrical Stimulation
Therapy to Heal Pressure Injuries. Wound Management & Prevention.
2020;66(1):14-23.
44. Peisah C, Lerman Y, Herrmann N, Rezmovitz J, Shulman K. Piloting
the global capacity education e-tool: can capacity be taught to health care
professionals across different international jurisdictions? International
Psychogeriatrics. 2021;33(9):913-6.
45. Roberts S, Chankitwanit N, Schwaba J, Schallert MC. Lessons Learned
from the Critical Illness Network: Implementing Evidence-Based Dietetics
Practice. Support Line. 2011;33(2):22.
46. Sarkies MN, Maloney S, Symmons M, Haines TP. Video strategies
improved health professional knowledge across different contexts: a helix
counterbalanced randomized controlled study. Journal of Clinical
Epidemiology. 2019;112:1-11.
47. Scrivener K, Akkermans J, Svanetti S, Szilas C, Robson M, Love S.
Examining user perspective of an online learning resource for
physiotherapists: A mixed methods study of the TRAIN program. Physiotherapy
Research International. 2021;26(3):e1917.
48. Swords C, Bergman L, Wilson-Jeffers R, Randall D, Morris LL,
Brenner MJ, Arora A. Multidisciplinary Tracheostomy Quality Improvement in
the COVID-19 Pandemic: Building a Global Learning Community. Annals of
Otology, Rhinology & Laryngology. 2021;130(3):262-72.
49. Robitaille E, MacRae M, Rowe P, Aiken A. A knowledge translation
intervention to promote evidence-based practices in ankle sprain management
among Canadian Armed Forces physiotherapists: Six-month results. Journal of
military, veteran and family health. 2021;7(1):46-54.
50. Szekeres M, MacDermid JC. Online learning versus workshops: a rank
minimized trial comparing the effect of two knowledge translation
strategies designed to alter knowledge, readiness to change, and
self-efficacy with respect to rehabilitation outcome measures. Disability
and rehabilitation. 2022;44(21):6531-8.
51. Heitman K, Proaño GV, Papoutsakis C, Diaque Ballesteros P,
Steiber A, Taylor CA. Learning Outcomes From a Virtual Nutrition Care
Process Workshop Delivered to Nutrition and Dietetics Professionals in
Mexico. Topics in clinical nutrition. 2023;38(2):113-24.
52. Jorge AES, Bennell KL, Kimp AJ, Campbell PK, Hinman RS. An
e-Learning Program for Physiotherapists to Manage Knee Osteoarthritis Via
Telehealth During the COVID-19 Pandemic: Real-World Evaluation Study Using
Registration and Survey Data. JMIR medical education. 2021;7(4):e30378.
53. McGrath V. Reviewing the Evidence on How Adult Students Learn: An
Examination of Knowles' Model of Andragogy. Adult Learner: The Irish
Journal of Adult and Community Education. 2009;99:110.
54. Atkins L, Francis J, Islam R, O'Connor D, Patey A, Ivers N, Foy R,
Duncan EM, Colquhoun H, Grimshaw JM, Lawton R, Michie S. A guide to using
the Theoretical Domains Framework of behaviour change to investigate
implementation problems. Implementation science : IS. 2017;12(1):77.
55. Michie S, van Stralen MM, West R. The behaviour change wheel: a new
method for characterising and designing behaviour change interventions.
Implementation science : IS. 2011;6(1):42.
56. Imms C, Kerr C, Bowe SJ, Karlsson P, Novak I, Shields N,
Reddihough D, Best Service Best Time Author Group. Knowledge translation
for allied health professionals working with children with cerebral palsy:
effects on evidence-based knowledge and practice. Physiotherapy.
2016;102:e35-e36.
57. Hitch D, Pepin G, Lhuede K, Rowan S, Giles S. Development of the
Translating Allied Health Knowledge (TAHK) Framework. International Journal
of Health Policy and Management. 2019;8(7):412-23.
58. Levac D, Glegg SMN, Camden C, Rivard LM, Missiuna C. Best practice
recommendations for the development, implementation, and evaluation of
online knowledge translation resources in rehabilitation. Physical Therapy.
2015;95(4):648-62.