Health Education in Practice: Journal of Research for Professional Learning
Vol. 7 | No. 1 | 2024
Education-in-practice article (single blind peer-review)

Copyright is held by the authors with the first publication rights granted to the journal. Conditions of sharing are defined by the Creative Commons License Attribution-ShareAlike-NonCommercial 4.0 International
Citation: Delaney, AM, Duffield, JA, Iten, R, Heywood, M, McLarty, AM & Bowers, AP 2024, ‘An education model for paediatric palliative care’, Health Education in Practice: Journal of Research for Professional Learning, vol. 7, no. 1 https://doi.org/10.33966/hepj.7.1.17855
An education model for paediatric palliative care
Angela M Delaney  1,6, Julie A Duffield
1,6, Julie A Duffield  2, Rebecca Iten
2, Rebecca Iten  3, Melissa G Heywood
3, Melissa G Heywood  4, Alison M McLarty
4, Alison M McLarty  1,6, Alison P Bowers
1,6, Alison P Bowers 5,6
5,6
Abstract
Introduction:
Meeting the palliative care needs of children and their families is
complex and challenging. For countries such as Australia, whose
relatively small paediatric palliative care population is dispersed
across a very large geographical area, one challenge is maintaining a
skilled workforce in regional, rural, and remote areas, where, when
compared to major cities, there are fewer resources, and the workforce
is often transient.
Methods:
The Quality of Care Collaborative Australia (QuoCCA) Pop-up Model of
Education was used to provide palliative care education to health
professionals across three geographical locations and facilities, to
facilitate a 2,500-km transfer of a child with complex palliative care
needs from a tertiary hospital to the remote family home on
Country.
Results:
Each Pop-Up provided effective education to facilitate the successful
transfer of the child to the next hospital location. Over 18 months,
three Pop-Ups occurred. Relational learning and real-time problem
solving enabled health professionals to build confidence and capacity
to successfully transfer the child from the regional hospital to the
remote family home.
Implications:
The QuoCCA Education Pop-up Model is a feasible method to deliver
timely access to speciality education. The model can be successfully
applied in multiple settings.
Keywords:
paediatric, palliative care, integrated health care delivery, learning,
rural, education models.
1 Paediatric Palliative Care Service, Children's Health
Queensland Hospital and Health Service, Brisbane, Australia
2 Paediatric Palliative Care Service, Women's and Children's
Health Network, Adelaide, Australia
3 Paediatric Palliative Care Service, Perth Children's Hospital,
Perth, Australia
4 Victorian Paediatric Palliative Care Program, Royal Children's
Hospital, Melbourne, Australia
5 Cancer and Palliative Care Outcomes Centre, Centre for
Healthcare Transformation, Queensland University of Technology, Brisbane,
Australia
6 Centre for Children's Health Research, Queensland University
of Technology, South Brisbane, Australia
Corresponding author: Angela M Delaney, Queensland
Children's Hospital, 501 Stanley Street, South Brisbane, Queensland, 4101,
Australia,
[email protected]
INTRODUCTION
Over the past two decades, specialist paediatric palliative care (SPPC)
services have grown globally (Ekberg, Bowers & Bradford 2021). As the
need and demand for SPPC continues to grow faster than the specialist
workforce, it is imperative that alternative models of SPPC education are
explored to ensure that high quality, well-coordinated family-centred care
is delivered in the right place at the right time (Mherekumombe 2018).
Compared to the adult population, the paediatric palliative care population
is relatively small and often geographically dispersed. The combination of
the complexity of the child's condition and intricacies of health systems
makes delivery of paediatric palliative care challenging (Bowers et al.
2020). Delivery of such care in areas where there are less resources and
fewer service providers can add further complexity (Queensland Health
2019).In Australia, the distance and diverse terrain between
major cities, where SPPC services are based, and regional, rural and remote
areas where families live is an additional challenge to timely palliative
care (Dassah et al. 2018).Children receiving palliative care
present with varying considerations including rarity of diagnoses,
developmental considerations, complex symptom management and the
psychosocial implications of family-centred care (Bowers et al. 2020).
In 2015, the Quality of Care Collaborative Australia (QuoCCA) project, a
nationally funded collaboration of interdisciplinary services, was
established to deliver paediatric palliative care education to health
professionals across Australia who may care for children with palliative
and end-of-life care needs. The aim of this national collaborative is to
'improve the quality of palliative care provided to children in close
proximity to their home, throughout Australia through innovative
education.' (CareSearch & QuoCCA 2018). The Commonwealth Department of
Health and Aged Care National Palliative Care Projects has continued to
fund the QuoCCA project through to June 2026.
METHOD
The QuoCCA project was conducted in collaboration with the five state-wide
SPPC services. The aim was to ensure education was delivered to health
professionals caring for children with life-limiting conditions across
Australia and the families of the children. Ethical approval was obtained
from the Children's Health Human Research Ethics Committee. Informed
consent was obtained verbally and in written form from the participant in
this report. This paper uses Jo's (pseudonym) 18-month journey to describe
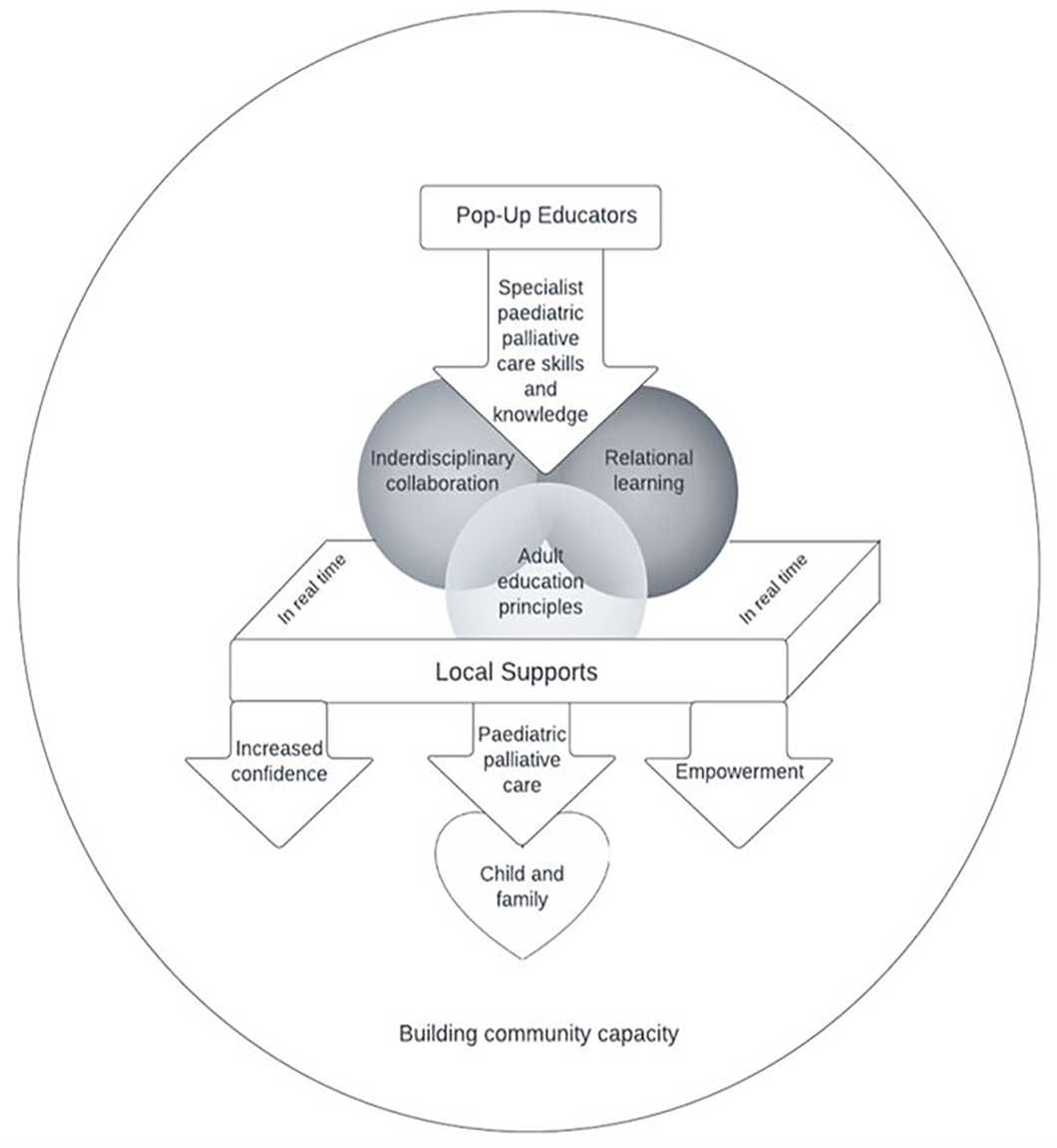
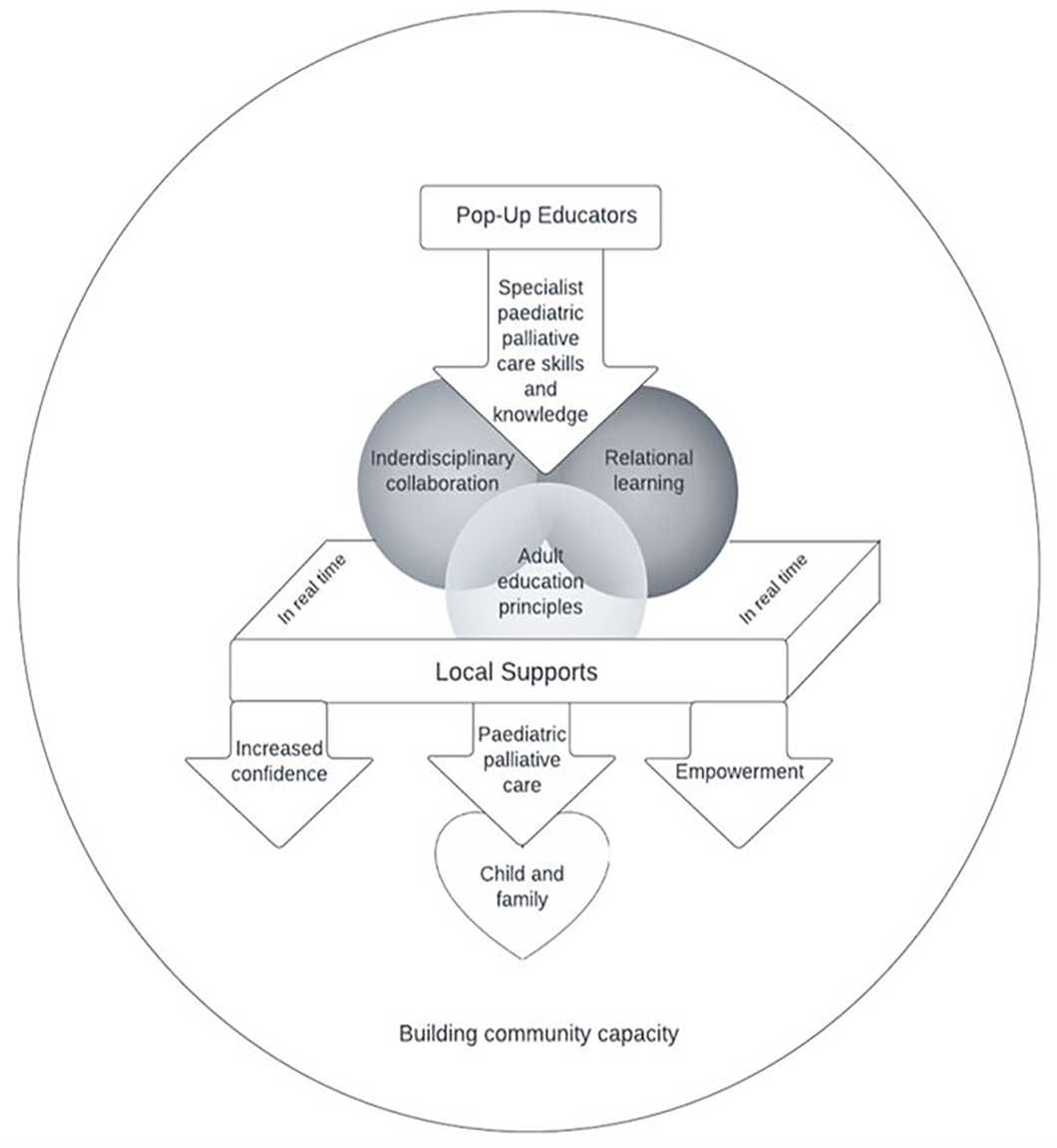
the QuoCCA Education Pop-Up Model for Paediatric Palliative Care (QE-PMOC)
(Figure 1) in practice. The QE-POMC aligns with central tenets of the
public health approach to palliative care, as it encourages collaboration
between acute and community services, supports the creation of supportive
environments and helps strengthen community action (Rosenberg, Mills &
Rumbold 2016).
Figure 1. QE-PMOC. This model is designed to deliver paediatric palliative
care education that facilitates collaboration and capacity building.
The Pop-Up Model
A Pop-Up is described as 'a specific intervention over and above care
that is provided to a child and family, with identified goals,
objectives and interventions leading towards improving the confidence
of local health care providers to deliver paediatric palliative care'
(Mherekumombe et al. 2016; Mherekumombe 2018). The QuoCCA project has
developed the QE-PMOC with other key enablers using the principles of
Pop-Up education (Table 1) to deliver education to individuals involved
in the care of the child and their family. These key enablers are
central to the development of the education while allowing for
flexibility of delivery.
Jo's case is used to illustrate how the QE-PMOC is implemented to deliver
effective palliative care education, resulting in the collaboration and
capacity building of health professionals.
Table 1: Key enablers for Pop-Up education
|
Key Enablers
|
Definition
|
|
Adult learning principles
|
Enhance the transfer of knowledge and understanding for
health professionals providing patient care.
1. Need to know
2. Self-concept
3. Prior experience
4. Readiness
5. Learning orientation
6. Motivation to learn
|
|
Relational learning
|
Learning via vicarious lived experience enhances a deeper
understanding of the child and family's lived experience.
|
|
Real time
|
At the time of care delivery, tailoring topics to
learners' needs in relation to the specific care issues of
the patient and family.
|
|
Local champion
|
Local champions are the point of contact health
professionals who take responsibility for the facilitation
and coordination of care, and education sessions to other
health professionals, conveying the family's goals of
care.
|
(Browning & Solomon 2006; Slater, Osborne & Herbert 2021; Adult
Learning Australia 2024)
THE CASE OF JO
Jo, an Aboriginal Australian, was born prematurely. Jo had multiple health
complications and co-morbidities that would shorten life expectancy. Jo's
family live in a remote community over 2,500 km from the tertiary health
service where Jo was an admitted patient. It was of cultural importance
that Jo and family lived on
Country[1]. Although Jo's life expectancy
remained shortened, several months later, Jo's condition was stable enough
to consider a transfer to a hospital on Country closer to the family's
community.
RESULTS
Due to the vast distance and remote terrain between the tertiary hospital
and Jo's community, Jo's transfer home required three Pop-Up education
sessions over a period of two years. The first transfer was from the
tertiary hospital to a small remote hospital >1,000 km from the family
home.
The first Pop-Up
The SPPC Nurse Educator (NE) and the Regional Adult Palliative Care Service
(RAPCS) visited the child and family in the remote hospital within a month
of the first transfer. The first Pop-Up occurred during this initial visit.
Education Topics
Many staff in rural or remote hospitals have never cared for a child with
palliative care needs; therefore, it is important that the professionals
involved identify the topics relevant to their learning needs in caring for
the patient and family. The health professionals caring for Jo experienced
moral and ethical challenges, and identified general care, complex symptom
management and how to navigate moral and ethical challenges when delivering
best-practice palliative care as relevant topics.
The Local Champion
Identifying a 'local champion' is an important element of facilitating a
Pop-Up. The SPPC NE engaged the RAPCS Aboriginal Health Worker (AHW), who
already had an established relationship with the family, and understood
their need for culturally safe care, to help coordinate and facilitate
group and one-to-one education sessions at the rural hospital.
Relational Learning In Real Time
The collaboration between the AHW and the SPPC NE facilitated the delivery
of education sessions that met the needs of the health professionals and
the culturally safe holistic care of the family in real time. This enabled
health professionals and the family to be supported as they navigated
decision-making and care interventions.
The second and third Pop-Up
In Jo's case there were two more Pop-Ups to facilitate subsequent
transfers. Local champions were identified from each hospital and worked in
partnership with each other, other health professionals, and the community
services that provided care to Jo and Jo's family.
For the second and third Pop-Up, topics and support provided by the SPPC NE
to health professionals were directed by each participating group, proving
similar to the learning needs of the previous group. At each transfer point
the SPPC NE provided Pop-Up face-to-face education, while the
interdisciplinary specialist paediatric palliative care service provided
support and guidance via telephone, email, and telehealth throughout all
stages of Jo's journey back to Country. During a Pop-Up visit, the SPPC NE
will often visit the patient in the family home. In Jo's case the SPPC NE
visited the family home and provided education to the support workers. The
number of stakeholders and interagency collaborations grew with each
transfer, building the capacity of clinicians across the geographical
expanse.
Throughout Jo's 18-month journey, the SPPC NE was supported, via the QuoCCA
project, to facilitate three in-person Pop-Ups which delivered education
and support to over 60 health professionals, from three acute service
providers (hospitals) and three community health services. Table 2
illustrates specific information related to each of the Pop-Up education
sessions.
Table 2: QE-PMOC Education Dataz
|
|
Pop-Up 1
|
Pop-Up 2
|
Pop-Up 3
|
|
Timeline
|
Oct 2018 & Feb 2019
|
June 2019 & Oct 2019
|
Nov 2020
|
|
Jo's age
|
4-6 months
|
12-14 months
|
2.5 years
|
|
Location
|
Hospital & adult palliative care service
|
Hospital
|
Health centre & family home
|
|
Facilitators
|
SPPC NE & clinical nurse consultant
|
SPPC NE
|
SPPC NE & medical fellow
|
|
No. of sessions
|
3
|
4
|
3
|
|
Mode of delivery
|
Face-to-face
|
One video conference & three face-to-face
|
Face-to-face
|
|
Total Pop-Up hours
|
6.25
|
6
|
6.5
|
|
Family session hours
|
3
|
3
|
1.5
|
|
Professionals:
Medical
Nursing
Allied Health
Support worker
Other
|
3
12
11
-
13
|
3
15
9
-
8
.
|
3
3
0
6
-
|
|
Total participants
|
36
|
35
|
12
|
Evaluation of Pop-Up education at the time included open-ended responses
from educators.
Across the three Pop-Ups, the NE reported consistent themes and suggested
successful outcomes which included increased inter-professional
collaboration, improved confidence and capacity building of local
professionals, and families trusting local teams following the tertiary
team working collaboratively with local services.
"Building this relationship has been vital. We were able support the team
in their decision making and symptom management of the patient." Nurse
educator (2019).
DISCUSSION
Through in-time professional education, interprofessional collaboration and
acknowledgment of the expertise of the family, the QE-PMOC successfully
built the capability, skills, knowledge and confidence of an
inter-professional care network, and increased the capacity of the local
community (Slater et al. 2018).
As demonstrated by Jo's case, the success of the QE-PMOC is reliant on
effective education via methods appropriate to the situation and learners'
needs (Browning & Solomon 2006; Curran & Sharpe 2007). The Pop-Up
education delivered at the time of care provision promoted in-time
interprofessional collaboration, and enabled questions to be addressed and
challenges to be overcome as they occurred.
Strengths
QE-PMOC education is learner-driven, with the child and family at the
centre, resulting in the right care in the right place at the right time
(Palliative Care Australia 2018). Furthermore, the QE-PMOC can help overcome
the challenge of location by taking specialist skills, knowledge, resources
and support from the tertiary centre to the family's local service
providers and community. The QE-PMOC supports the real-time sharing of
evidence-based best-practice paediatric palliative care in the family and
patient's choice of location and at the time of need, which mitigates local
health costs of travel for professional development.
Challenges and questions can be addressed in real time, enabling
professionals to confidently provide coordinated care (Mherekumombe 2018;
Slater et al. 2018). This facilitates effective communication between local
professionals and family members. Effective communication helps
professionals to build trust with families, and helps families build
confidence in the professional's ability to provide effective care, where
the family's knowledge and experience are valued and decision making is
shared (Stein et al. 2019).
In the experience of QuoCCA educators, the local champion is a role based
on the local team's understanding and value of an individual's experience,
skills, and any existing rapport with the family. The local champion is the
key link between the SPPC NE and local health professionals and has a key
role in advocating the views and wishes of the family and in coordinating
care (Department of Health and Aged Care 2022). Drawing on a
strengths-based approach (Miller 1990), the QE-PMOC facilitates reframing
what individuals feel they do not know and cannot provide, to what they do
know and can provide. Reflections of QuoCCA educators suggest that once a
QE-PMOC has been provided, local health care professionals delivering care
will confidently seek to contact the SPPC service, for reassurance,
guidance, and knowledge-sharing. This is supported by Sansone, Ekberg and
Danby (2022), who report that an SPPC provided reassurance to individuals
who called a SPPC help-line.
The model can be successfully applied in multiple settings, including in
areas with limited resources or service infrastructure. The model has the
potential to be used in specialities other than paediatric palliative care.
Limitations
Further research is needed to explore the impact of the QE-PMOC on health
professionals receiving education and on the families at the centre of the
intervention. The preparation time leading into a Pop-Up education event,
including topic preparation and coordination, has not been documented.
However, as activities associated with Pop-Up education are multi-layered
and cannot be viewed in isolation, quantifying the effects and impact of a
Pop-Up may be challenging. Despite these challenges, work is currently
underway to quantify such impacts and effects.
CONCLUSION
The QE-PMOC ensured that all professionals, services, and community members
received the education and support needed to plan and transition Jo's care
back to the family home and community. Australian SPPC educators consider
the QE-PMOC as the gold standard for improving equitable, accessible, and
quality paediatric palliative care. The QE-PMOC is a feasible method of
delivery of timely speciality education that meets the learning needs of
health professionals and the culturally safe holistic palliative care needs
of children and their families.
Acknowledgements
We would like to acknowledge and thank the family who agreed for this case
to be shared, and pay respects to their Elders, lores, customs and creation
spirits. We acknowledge the traditional owners of the lands where the
family live and where the Pop-Ups occurred. We recognise that these lands
have always been places of teaching, learning and research. We acknowledge
the important role Aboriginal and Torres Strait Islander people play within
our communities.
We would also like to acknowledge the contribution of Ashka Jolly, QuoCCA
NE for the Australian Capital Territory, and Sarah Baggio, Allied Health
Educator, and the contributions of the rest of the National QuoCCA project
team.
Conflicts of Interest and Source of Funding
No conflicts to declare. The QuoCCA project is funded by the Commonwealth
Department of Health and Aged Care through the National Palliative Care
Projects.
Ethics
This project received multi-centre ethics from the Children's Health
Queensland Human Research Ethics Committee reference HREC/16/QRCH/55. Both
verbal and written parental consent was obtained, as advised by HREC for
the use of this case.
Contributorship Statement
AD, JD and RI drafted the initial manuscript.
AB, AM, MH, AD, JD and RI made substantial contributions to interpretation
of the work, developed the model of care figure, and reviewed and
critically revised drafts of the manuscript for important intellectual
content. AD, JD, RI, MH, AM, and AB approved the final version for
publication.
REFERENCES
Adult Learning Australia 2024, The principles of adult learning,
viewed March 2024,
https://ala.asn.au/adult-learning/the-principles-of-adult-learning/
Australian Institute of Aboriginal and Torres Strait Islander Studies 2022,
Welcome to country, viewed 19 October 2022,
https://aiatsis.gov.au/explore/welcome-country#
Bowers AP, Chan RJ, Herbert A, Yates P 2020, 'Estimating the prevalence of
life-limiting conditions in Queensland for children and young people aged
0-21 years using health administration data',
Australian Health Review
, vol. 44, pp. 630-6. DOI: 10.1071/AH19170.
Browning DM & Solomon MZ 2006, 'Relational learning in pediatric
palliative care: Transformative education and the culture of medicine',
Child and Adolescent Psychiatric Clinics of North America, vol.
15, pp. 795-815, DOI: 10.1016/j.chc.2006.03.002.
CareSearch & the QuoCCA project 2018,
Quality of Care Collaborative Australia
(QuoCCA), viewed 19 October 2022,
https://www.quocca.com.au/default.aspx
Curran VR & Sharpe D 2007, 'A framework for integrating
interprofessional education curriculum in the health sciences',
Education for Health (Abingdon, England),
vol. 20, pp. 93.
Dassah E, Aldersey H, McColl MA & Davison C 2018, 'Factors affecting
access to primary health care services for persons with disabilities in
rural areas: A "best-fit" framework synthesis',
Global Health Research and Policy
, vol. 3, pp. 36. DOI: 10.1186/s41256-018-0091-x.
Department of Health and Aged Care 2018,
The national palliative care strategy
, viewed 19 October 2022,
https://www.health.gov.au/resources/publications/the-national-palliative-care-strategy-2018
Ekberg S, Bowers A, Bradford N, Ekberg K, Rolfe M, Elvidge N, Cook R,
Roberts SJ, et al. 2021, 'Enhancing paediatric palliative care: A rapid
review to inform continued development of care for children with
life‐limiting conditions', Journal of Paediatrics and Child Health
, vol. 58, pp. 232-7. DOI: 10.1111/jpc.15851.
Mherekumombe MF 2018, 'From inpatient to clinic to home to hospice and
back: Using the "pop up" pediatric palliative model of care',
Children (Basel)
, vol. 55, no. 5, pp. 55. DOI: 10.3390/children5050055.
Mherekumombe M, Frost J, Hanson S, Shepherd E & Collins J 2016, 'Pop
Up: a new model of paediatric palliative care',
Journal of Paediatrics and Child Health
, vol. 52, pp. 979-82. doi.org/10.1111/jpc.13276
Miller GE 1990, 'The assessment of clinical skills/competence/performance',
Academic Medicine, vol. 65, S63-7, DOI:
10.1097/00001888-199009000-00045.
Palliative Care Australia 2018,
Palliative care service development guidelines
, viewed 19 October 2022,
http://palliativecare.org.au/wp-content/uploads/dlm_uploads/2018/02/PalliativeCare-Service-Delivery-2018_web2.pdf
Queensland Health 2019,
Queensland health palliative care services review: Key findings
, viewed 19 October 2022,
https://www.health.qld.gov.au/__data/assets/pdf_file/0025/852622/palliative-care-services-review-key-findings.pdf
Rosenberg JP, Mills J & Rumbold B 2016, 'Putting the 'public' into
public health: Community engagement in palliative and end of life care',
Progress in Palliative Care, vol. 24, pp. 1-3. DOI:
10.1080/09699260.2015.1103500.
Sansone HM, Ekberg S & Danby S 2022, 'Uncertainty, responsibility, and
reassurance in paediatric palliative care: A conversation analytic study of
telephone conversations between parents and clinicians',
Qualitative Health Communication
, vol. 1, pp. 26-43, DOI: 10.7146/qhc.v1i1.125538.
Slater PJ, Herbert AR, Baggio S, Donovan LA, McLarty AM, Duffield JA,
Pedersen LC, Duc JK, et al. 2018, 'Evaluating the impact of national
education in paediatric palliative care - The Quality of Care Collaborative
Australia', Advances in Medical Education and Practice, vol. 9,
pp. 927-41. DOI: 10.2147/AMEP.S180526.
Slater PJ, Osborne CJ & Herbert AR 2021, 'Ongoing value and practice
improvement outcomes from pediatric palliative care education: The Quality
of Care Collaborative Australia',
Advances in Medical Education and Practice
, vol. 12, pp. 1189-98. DOI: 10.2147/AMEP.S334872.
Stein A, Dalton L, Rapa E, Bluebond-Langner M, Hanington L, Stein KF,
Ziebland S, Rochat T, et al. 2019, 'Communication with children and
adolescents about the diagnosis of their own life-threatening condition',
The Lancet, vol. 393, pp. 1150-63, DOI:
10.1016/S0140-6736(18)33201-X.
[1]Country is the term often used by Aboriginal peoples to describe
the lands, waterways, and seas to which they are connected. The
term contains complex ideas about law, place, custom, language,
spiritual belief, cultural practice, material sustenance, family,
and identity (Australian Institute of Aboriginal and Torres Strait
Islander Studies, 2022).