Evaluating the impact of the Assistant in Medicine (AiM) program on medical workforce efficiency and preparedness in NSW, Australia
Alicia B Mitchell ![]() 1,2,3, Hilary Parsons
1,2,3, Hilary Parsons ![]() 1,2, Hemal Patel
1,2, Hemal Patel ![]() 1,2,4
1,2,4
Abstract
The Assistant in Medicine (AiM) program allows selected final-year medical students to take on more responsibility while also supporting the junior doctor workforce. This study aimed to evaluate the impact of the AiM program on current medical staff, including junior doctors, registrars and consultants working in public teaching hospitals on NSW's Central Coast. Furthermore, it aimed to investigate the effect of this AiM program on final-year medical students, their learning and the transition to internship. This cross-sectional study surveyed a select group of 75 medical officers and all 28 final-year medical students employed as AiMs on the Central Coast during July- September 2023. Of the medical officers surveyed, 53.3% felt that they were able to see more, or substantially more, patients on a shift where they had an AiM present and 71.8% felt that a shift with an AiM present was more or substantially more enjoyable than one without. Our results also show that the AiM program allowed doctors to focus on higher-level tasks and to find more enjoyment in their shifts, which may be beneficial in reducing the high rates of burnout seen in the current junior doctor cohort. The entire cohort of student respondents indicated that the AiM position helped them to feel more prepared for internship, with 95% feeling more integrated into the team, indicating enhanced clinical readiness. Furthermore, this study indicates that all the final- year medical students participating in the AiM program on the Central Coast found the program to be beneficial to their learning, increasing their exposure to clinical skills and better preparing them for internship. Limitations of this study include a low response rate from doctors working in the local health district and the limited ability to explore qualitative data within the current study design.
Keywords: assistant in medicine, junior doctor, workforce shortage
1 Central Coast Local Health District, Gosford, Australia
2 Central Coast Clinical School, School of Medicine and Public Health, University of Newcastle, Gosford, Australia
3 UNSW Medicine and Health, University of New South Wales, Randwick, Australia
4 New South Wales Ambulance, Sydney Olympic Park, Australia
Corresponding author:Dr Alicia B Mitchell, Central Coast Clinical School, School of Medicine and Public Health, University of Newcastle, Gosford NSW 2250, Australia, [email protected]
INTRODUCTION
The Assistant in Medicine (AiM) program has allowed eligible final-year medical students to take on more responsibility while also supporting the junior doctor workforce. The AiM role was developed in March-April 2020 as part of New South Wales (NSW) Health COVID-19 medical surge workforce planning and was designed to supplement the existing junior medical workforce. This was a voluntary opt-in position with up to 32 working hours per week, where AiMs were employed by NSW Health and paid at 75% of the NSW medical intern salary. The AiM program continued after the COVID pandemic as a way of supporting the junior doctor workforce, which is facing critical workforce shortages and high levels of burnout. The 2022 Australian Medical Association (AMA) Hospital Health Check for NSW indicated that 72% of junior doctors reported working more than 5 hours of unrostered overtime per fortnight, a significant increase from 49% in 2020. In addition, 46% of junior doctors reported making a fatigue-induced error and 56% indicated their concern for their safety due to fatigue from working long hours (AMA 2022). The Australian College of Emergency Medicine reports that staff shortages are becoming self- perpetuating, with more skilled staff leaving due to unsustainable working conditions, leading to worsening of the current staffing crisis (ACEM 2023). It is imperative that the Australian health care system continues to find strategies to deal with the workforce shortages, particularly in the junior doctor cohort that make up the bulk of the hospital medical workforce.
While existing research has demonstrated workforce improvements with interventions similar to the AiM program, few have quantitatively assessed both staff satisfaction and student readiness within the same framework, particularly in the context of NSW's unique healthcare challenges. This study aimed to quantitatively evaluate both the immediate operational benefits and the educational impacts of the AiM program, providing a dual perspective on its efficacy. It aimed to do this through 1) determining the impacts of the program on current medical staff, including junior doctors, registrars and consultants working at Gosford and Wyong public teaching hospitals on NSW's Central Coast; and 2) investigating the effect of the local AiM program on final-year medical students, their learning and transition to internship.
METHODS
This practical cross-sectional observational study surveyed participants during July-September 2023. Responses were obtained from doctors (junior through to senior medical officers) and final-year medical students working at the Central Coast Local Health District (CCLHD), in NSW, Australia. Participants were recruited via a workforce-and/or university- distributed email, with informed consent gained prior to input in the survey. The surveys were sent to 557 medical officers and 28 medical students participating in the AiM program. A total of 75 doctors responded to the survey (13% response rate), while 100% of the final-year medical students working as part of the AiM program responded. A range of data including the number of hours worked, the specialty area that was worked in, the impact on learning and the impact on reduction of workload for doctors was recorded. Most responses were obtained via a Likert scale whereby doctors and medical students could rate the impact on their workload and learning; however, the opportunity for free-text answers was also provided in order to gain a greater understanding of individual responses to the program. Ethics approval as a low and negligible risk study was obtained from the CCLHD Research Office, with the approval number 0623-061C.
A five-point Likert scale was utilised to determine numerical responses ranging from substantially more (5) through to substantially less (1). For example, one of the Likert-scale questions asked respondents to answer the question: 'Did you feel that you could spend more time on higher-level tasks on a shift with an AiM?' Using a scale from 5 (substantially more) to 1 (substantially less). Responses were analysed and percentages were derived based on agreeance with the statement presented and mean values were calculated. Free-text responses were used to contextualise the responses gained via the Likert scale, and are presented as direct quotes to identify particular benefits or areas of improvement for the program.
RESULTS
CCLHD has employed AiMs since 2020, and was in its third year of the program when feedback was collected from medical officers and students regarding the impact of the program. The students were in their second semester of placement as an AiM at the time of survey, and were placed across medical and surgical teams and in the emergency department (ED). The placements were determined based on curriculum requirements, with students fulfilling standard placement requirements while working as an AiM. On those days (2 days per week) that the students did not have AiM employment, they were still expected to attend other specialty clinical placements and classroom teaching.
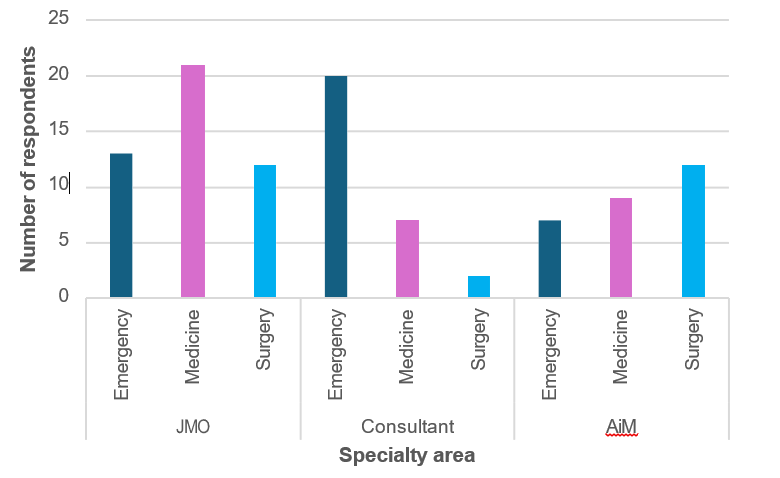
An online questionnaire was sent to all medical officers asking questions regarding the impact of AiMs on workload and workflow. In total, 75 responses (13% response rate) were received from junior and senior medical officers, in a range of specialty areas, as seen in Figure 1. A separate questionnaire was sent to all current students participating in the AiM program in the local health district, with 28 responses received (100% response rate). Students had been allocated to medical teams (32%, n = 9), surgical teams (43%, n = 12) and the ED (25%, n = 7) for a period of nine weeks. The questionnaires asked about the impact of the AiM program on student's education, learning, time management and readiness for internship.
Of the 75 medical officers that responded to the questionnaire, 29 (38%) responses were from senior medical officers, while 46 (62%) were from junior medical officers ranging from interns to senior registrars and from a range of acute care areas (Figure 2). Of those senior medical officers that responded, the majority worked in the ED (69%, n = 20) and may have had more direct interactions with AiMs than the senior medical officers working on the wards. Of those non-ED consultants that responded to the survey, seven were in medical specialties and two were surgical consultants. Of the junior doctors who responded to the survey, there was a more even spread of specialties represented with 46% working in medical specialties (n = 21), 26% in surgical specialties (n = 12) and 28% working in the ED (n = 13).
Figure 1: Position of doctors surveyed
Figure 2: Specialty area of medical officers and assistants in medicine
As seen in Table 1, medical officers reported a marked improvement in shift satisfaction and efficiency with AiMs. Specifically, of the 75 medical officers who responded, 53.3% noted they were able to see more patients, 62.8% reported a decreased workload, 71.8% felt that a shift with an AiM present was more or substantially more enjoyable than one without and 70.5% felt that they were able to spend more time on higher-level tasks with an AiM present (Figure 3). The effects were more apparent when the doctors were working in the ED, where 19 of 33 doctors surveyed (57%) reported a decreased or significantly decreased workload on shifts with an AiM. The workload decrease was strongest for consultants, where 13 of 20 ED staff specialists (65%) reported this effect. Interestingly, the perceived stress levels at the end of a shift with an AiM present were similar to those for shifts without an AiM. Comments from medical officers also indicated a positive effect on workload and efficiency from the presence of AiMs (Table 2). Overall, the comments indicated that, although some final-year medical students still required further teaching to fit well into the AiM role, they provided significant support to the junior doctor workforce, and that the program provided additional opportunities for the medical students to learn skills while on placement.
Table 1: Average responses from medical officers reflecting on working with AiMs
Statement |
Satisfaction(mean) |
Did you feel you were able to see more patients on a shift that had an AiM? |
3.60 |
Did you feel that you could spend more time on higher-level tasks on a shift with an AiM? |
3.92 |
Were you likely to leave work on time at the end of a shift when an AiM was present? |
3.48 |
How was your perceived stress at the end of a shift that had an AiM (compared to without)? |
2.63 |
Did you find your shift with an AiM more enjoyable? |
3.90 |
* 1 = substantially less; 3 = no change; 5 = substantially more
Figure 3: Distribution of responses from medical officers
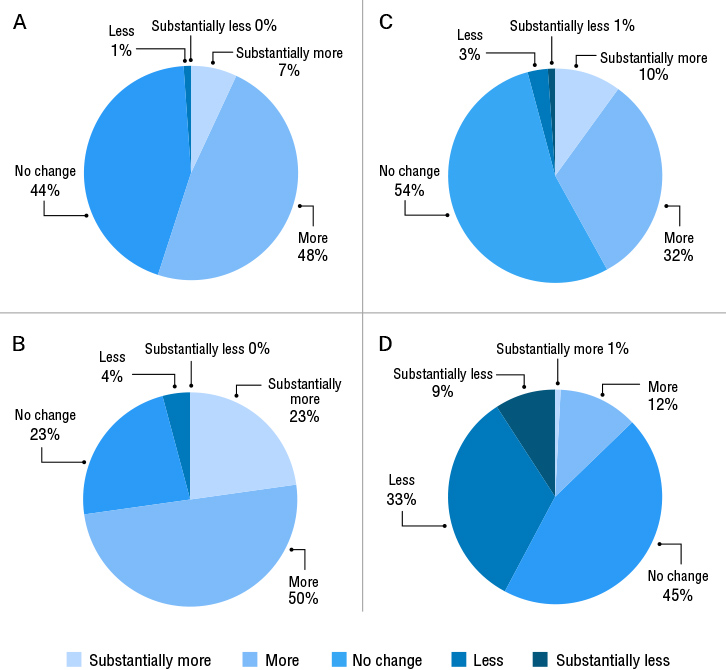 |
A: 'Did you feel you were able to see more patients on a shift that had an AiM?',
B: 'Did you feel that you could spend more time on higher-level tasks on a shift with an AiM?',
C: 'Were you likely to leave work on time at the end of a shift when an AiM was present?' and
D: 'How was your perceived stress at the end of a shift that had an AiM (compared to without)?'
Table 2: Example free-text responses from doctors
Question: Do you think that the use of final-year medical students as AiMs is a useful permanent addition to the medical workforce? |
Absolute genius. Assimilates them with the team whilst also providing them with purpose and risk appropriate roles. |
The AiMs ease the workload on clinicians and [the program] prepares the AiMs to slide into the intern role with ease. |
AIMs are an extremely valuable addition to the medical workforce. They have a huge impact on our workload and the enjoyability of our shifts. The position is also extremely beneficial to the continuing education of final- year medical students and prepares them very well for internship so they are able to hit the ground running and perform their jobs at the highest level. I worked as an AiM in the first year of their introduction and I am a better doctor for it, and I see the same with the interns coming through who worked as AiMs. |
Yes -as it allows them to become more competent and confident interns and interns also learn new things while teaching AiMs. Saves a great amount of time in ED and allows us to juggle more patients at once. As a side note, some consultants across different hospitals have noted that current interns have done fewer cannulas and blood procedures in ED compared to the years before AiMs and I am unsure of whether this would negatively impact JMO [junior medical officer] procedural skills in the long run due to lack of practice (as it used to be that ED term was the term for JMOs to hone their procedural skills through high volume of procedures - however it's also unclear if being deskilled in procedures is necessarily a bad thing as most registrars/consultants no longer do basic cannulas/bloods). |
The responses from students indicated that they found the AiM program to be beneficial, particularly in terms of learning practical skills to prepare them for internship and in terms of finding paid employment that was directly relevant to their training (Table 3). The AiMs were involved in performing a range of clinical tasks that will likely correlate directly with tasks they will be performing as interns (Table 4). This program also allows more time outside of clinical placement for study, rather than employment, for the students, as shown by the free-text responses in Table 5. These free-text responses capture the sentiment from the students that this program allowed them to integrate more fully into the clinical team and take on more responsibility, when compared with their usual medical school placements. All of the student respondents indicated that the AiM position helped them to feel more prepared for internship, and 95% of students felt more included in the medical team as an AiM than when on a standard medical student placement. There was an overwhelming majority vote that the AiM program was an easier way to source paid work, compared with other jobs that students had worked during medical school (89%).
Table 3: Average responses from AiMs reflecting on their roles
Statement |
Satisfaction(mean)* |
Do you think that the role has made you feel more prepared for starting work as an intern? |
4.64 |
Do you think that you learnt more in this AiM role than in medical student clinical placement? |
4.04 |
Do you feel that you were more involved with the team as an AiM compared to being a medical student? |
4.6 |
Do you feel that you had more opportunities to perform clinical skills as an AiM? |
4.21 |
Do you feel that you had the time and opportunity to meet your educational requirements whilst working as an AiM? |
3.7 |
*1 = substantially less; 3 = no change; 5 = substantially more
Table 4: Tasks completed by AiMs during shifts
Task |
Number reporting performing task |
Assisting in outpatient clinics |
3 |
Assisting in operating theatres |
7 |
Simple suturing |
2 |
Urinary catheterisation |
3 |
Patient admissions |
3 |
Clinical handover of patients |
11 |
Assessing hydration status |
16 |
Ordering/organising radiology investigations |
10 |
Ordering pathology investigations |
27 |
Organising consults |
28 |
Scribing during ward rounds |
23 |
Medical record documentation |
27 |
Performing cannulation |
22 |
Performing venepuncture |
22 |
Preparing discharge summaries |
24 |
Table 5: Example AiM free-text responses to survey questions
Question: How do you feel the role differed from the experience provided by clinical placement? |
Felt more like part of the team, and the team wasn't worried about giving me extra jobs. A good way to see how the junior doctors prioritise and distribute the tasks. Still found opportunities to partake in consultations/ surgeries for my own learning. |
I felt like I had more responsibility and was more a part of the team. I also felt I could help out more easily and knew what jobs I could do which would most help the team. |
Doing the AiM program allows us to get much more involved with patient care and therefore learn more about being an intern and working with a team. |
Question: Do you think this is an easier way for you to source paid work, compared with other jobs that you have worked during medical school? |
The organisers of [the] AiM program for the Central Coast are very organised and aligned AiMs' shifts with clinical placements, allowing us to fulfil uni requirements while also working. This meant we could focus on training for next year with less worry about having to earn a wage outside of medicine, and allowed us to use more of our free time for study or wellbeing activities other than work. This helped me to avoid burnout. |
Definitely. It's relevant to what we're learning so the time feels better spent and also counts towards placement hours. Having a different casual job would mean working after hours/night time and weekends, which affects study time. |
I definitely agree, placement and university hours take up a lot of our time during the week, which makes sourcing a paid job difficult as our availability is reduced. The things and skills we learn during the AiM program are also applicable to our internship which makes it a useful job to have. |
DISCUSSION
The results from this study show that the AiM program, in our centre, allowed doctors to see more patients during a shift and focus on higher- level tasks. The AiMs also provided back-up to the existing junior doctor workforce that is facing a critical shortage. The responses indicated that doctors found shifts with an AiM present more enjoyable, which may be beneficial in reducing the high rates of burnout seen in the current junior doctor cohort. Furthermore, this study indicates that all of the final-year medical students participating in the AiM program on the Central Coast found the program to be beneficial to their learning, increasing their exposure to clinical skills and better preparing them for internship. This is one of the largest independent studies to date that includes feedback from both medical officers and the medical students participating in the AiM program.
In 2023, when this study was being carried out, CCLHD had its largest cohort of AiMs so far, with 100% of all final-year medical students placed at the Central Coast Clinical School participating in the program. All students worked between 24 and 30 hours per week in this role and were matched to their university clinical rotations to ensure an immersive experience and to protect their curriculum based-learning activities. A minimum of 24 hours of employment per week ensured that students were attached to their clinical team for at least three full working days, which enabled integration and the ability to become familiar with the tasks that they carried out. Kolb's experiential learning theory (Kolb, 1984) posits that skills developed in a real-world context, such as those provided by the AiM program, are more deeply internalised, explaining the high levels of student preparedness observed.
These findings are reflected by the results of other AiM literature. The NSW Health Assistant in Medicine Evaluation Report (NSW Health 2021) found similar feedback about the benefits of the program from the 414 JMOs and 174 senior medical officers (SMOs) who responded. Feedback was overwhelmingly positive about the impact that AiMs had on team functioning, particularly in areas where they were able to provide relief from high levels of JMO vacancies in rural and regional hospitals that usually operate with less medical staff than metropolitan hospitals. Over a quarter (26%) of JMOs who responded to the survey stated that having AiMs on the team changed their roles and responsibilities and often allowed them to see more patients, attend theatre more frequently and practice to the highest end of their scope. Nearly half (47%) of JMOs who responded to the survey questions reported that AiMs decreased their workload and the most significant decrease was found to be where AiMs worked four days per week. As many as 76% of JMOs responding to the survey indicated that the AiM in their team functioned differently from a medical student on clinical placement and over 50% of SMOs responding to the survey echoed this. Clear parameters around the AiM role allowed medical officers to feel empowered to delegate tasks to AiMs.
A pilot study investigated the impact of AiMs in the ED (Rupasinghe, Majeed Omar & Berling 2023) in Newcastle, Australia. At the conclusion of each AiM shift, the supervising doctor completed an online questionnaire about their experience. Forty-seven survey responses were completed, corresponding to eight AiMs completing 47 shifts. Most doctors found that AiMs increased their productivity during a shift with 77% seeing more patients than they would on a normal shift. Furthermore, there were positive impacts on wellbeing with 100% of doctors finding their shifts enjoyable and 64% feeling less stressed at the end of a shift. Our study built on this data, looking at the impact of a greater number of AiMs across different specialty areas. We found similar outcomes, in that doctors felt the presence of AiMs increased their productivity and feeling of wellbeing at the end of a shift. Our study adds to the literature, as it also provides feedback from the perspective of the final-year medical students, and indicates that pursuing an AiM position is beneficial to them in a multitude of ways. Students felt more included and supported as part of the medical team, on the wards and in the ED, when employed in a formalised position by the hospital. The program helped to bridge gaps in administrative knowledge and skills, while teaching medicine's undocumented curriculum -knowledge that is essential for working as a junior doctor but is often excluded from medical school syllabi. Examples of the hidden curriculum include professionalism and ethics, communication skills, time management and prioritisation, navigating uncertainty and ambiguity, and interprofessional collaboration. Learning these aspects of the undocumented curriculum better prepares students for the complexities of clinical practice and promotes professionalism, empathy, and resilience among future healthcare providers.
Most Australian and New Zealand medical schools offer final-year medical students intensive pre-internship (PRINT) terms, of varying lengths, to more practically prepare students for commencing internship. A number of studies have evaluated these programs and have shown benefits for medical students in terms of ability, knowledge and confidence, particularly in the areas of procedural skills and operational management (Dare et al. 2009; McKenzie & Mellis 2017; Scicluna et al. 2014). To our knowledge, there are no studies that directly compare PRINT terms with the AiM program; however, in the case of the medical students participating in the AiM program at our centre, this placement was of a longer duration and more intensive than most PRINT terms described and offered an additional benefit to the students of being a paid placement, which has benefits in alleviating financial strain on the students. Furthermore, the AiM program presents some similarities to the workplace-based assessment (WBA) program offered to certain international medical graduates (IMGs) commencing work in Australia, in that skills are learned and assessed on the job and that the programs allow workforce shortages to be filled in the interim (Parvathy et al. 2021). Students on the AiM placement have a log book showing patient care-related and procedural tasks that need to be completed alongside regular clinical assessment tasks in order to successfully complete the rotation. This is similar to IMGs completing the WBA program (Nair et al. 2021). Many studies have demonstrated the efficacy of learning while on the job (Baboolal & Singaram 2023; Cave et al. 2009), and thus the AiM program may present some added benefits over a traditional intensive PRINT program.
The formalisation of the medical student apprenticeship role allowed for paid work experience and therefore contributed to medical students' financial wellbeing, with many stating that they no longer had to source work elsewhere. 'Placement Poverty' (Thorne 2024) is a neologism that describes the financial, emotional and physical burden on students who have to complete unpaid placements in order to achieve their qualifications. In May 2024, the Australian Government announced steps to address placement poverty for teaching, nursing and social work students with a means-tested payment available from July 2025 (Duffy 2024). There has been no mention of placement financial support for medical students who, on average, spend two years, or half of their degree, in unpaid placements. Our study shows that paid work experience via the AiM program results in positive financial, mental and physical health implications for medical students. The AiM program allows student to use their time outside of university placements, lecture and study requirements, for activities of daily living (eating, sleeping, cooking, cleaning), self-care, exercise and socialising, all of which are conducive to overall wellbeing and help to build more resilient healthcare professionals with better workplace retention (Mirza et al. 2021; Molodynski et al. 2021; Rajapuram et al. 2020).
The limitations of this study include the study design and the limited response rate. Firstly, the use of a survey-based design which captures attitudes of participants at only a single point in time, with most data being collected via visual analogue scales with minimal ability to expand further on these themes, may have restricted the ability for respondents to accurately describe their experience. However, the data was collected contemporaneously while AiMs were in the middle of their second placement for 2023, likely reducing recall bias in this setting. Secondly, the low (13%) response rate from the medical officers that were invited to participate may have implications of selection bias, as those who responded may have had stronger attitudes towards the program than those who did not participate in the study. The low response rate may be due to a number of factors, including a lack of time to complete the questionnaire due to competing clinical demands, survey fatigue due to the large number of surveys and feedback forms disseminated to doctors, or the nature of inviting participants via a workforce-distributed email to a work email address. The majority of SMO feedback was provided by consultants working in the ED, which may have skewed the data received to be less relevant to AiMs that were working in a ward-based setting. However, this may also reflect the nature of direct supervision in the different settings, as in the ED, consultants are directly involved in directing the day-to-day activities of the AiMs, while on the ward, JMOs have more direct interactions with the AiMs.
Furthermore, there was only limited qualitative data obtained using the comment boxes attached to questions in the questionnaire. This could be expanded on and explored further by the use of qualitative methods, such as interviews and audio diaries, as suggested by Monrouxe et al. in their evaluation protocol (Monrouxe et al. 2021). These methods could assist in gaining further information from both doctors involved in the program and the AiMs to determine the impacts on day-to-day workload and to determine ways to improve the program to make it more useful for filling the workforce shortages.
In terms of future directions from this study, a more in-depth qualitative study of the themes that have arisen would be useful. In addition, a larger study with more feedback from medical officers at both the junior and senior level and across disciplines would be useful to allow sufficiently powered statistical analyses of the data to present more robust conclusions regarding the overall impacts of this program.
CONCLUSION
The AiM program had a range of positive benefits for doctors and final-year medical students within the CCLHD workforce. This data is limited by the study design, low response rate, and potential selection bias; however, it presents further supporting evidence for the positive impacts of the AiM program on both medical professionals and medical students. Australia is facing healthcare worker shortages in the post-COVID era. AiMs are well- placed to play a role in filling the gaps of skilled labour within specific healthcare settings, including as parts of inpatient medical and surgical teams and in the ED, assisting with triaging and basic workup of patients. Many senior clinicians in our study commented that AiMs were taking the burden of simple tasks off junior doctors and thus contributing towards the team's overall productivity and workload. There are positive implications of this for stress levels and workplace enjoyability/satisfaction for doctors, which aligns with the Australian National Medical Workforce Strategy (Australian Government, 2024) and promotes doctor retention within the medical workforce. Furthermore, this study highlights benefits for the final-year medical students who participated in the AiM program, including the alignment of paid placement initiatives with the medical curriculum, fostering accountability and responsibility, and allowing the students to better integrate into clinical teams. This program encourages a seamless transition from medical school to internship, which provides further benefits to the workforce in an already strained medical system.
References
ACEM 2023, Doctor shortages in emergency departments set to worsen in 2023 , Australian College for Emergency Medicine, viewed 30 January 2025, https://acem.org.au/News/January-2023/Doctor-shortages-in-emergency- departments-set-to-w
AMA 2022, AMA (NSW) Hospital Health Check, AMA (NSW), viewed 6 April 2024, https://www.amansw.com.au/hhc-2022-hospital-grades/
Australian Government 2024, National Medical Workforce Strategy 2021-2031, Department of Health and Aged Care, viewed 16 February 2025, https://www.health.gov.au/our-work/national-medical-workforce- strategy-2021-2031
Baboolal, SO & Singaram, VS 2023, 'Specialist training: workplace-based assessments impact on teaching, learning and feedback to support competency-based postgraduate programs', BMC Medical Education , vol. 23, no. 1, p. 941.
Cave, J, Woolf, K, Jones, A & Dacre, J 2009, 'Easing the transition from student to doctor: how can medical schools help prepare their graduates for starting work?', Medical Teacher, vol. 31, no. 5, pp. 403-408.
Dare, A, Fancourt, N, Robinson, E, Wilkinson, T & Bagg, W 2009, 'Training the intern: The value of a pre-intern year in preparing students for practice', Medical Teacher, vol. 31, no. 8, pp. e345-350.
Duffy, C 2024, 'Budget relief for nursing and teaching students hit by "placement poverty."', ABC News, 5 May 2024, viewed 12 May 2024, https:// www.abc.net.au/news/2024-05-05/placement-poverty-commonwealth- payment-nurses-teachers/103807024
Kolb, DA (1984) Experiential learning: Experience as the source of learning and development , Prentice Hall, Englewood Cliffs NJ.
McKenzie, S & Mellis, C 2017, 'Practically prepared? Pre-intern student views following an education package', Advances in Medical Education and Practice , vol. 8, pp. 111-120.
Mirza, AA, Baig, M, Beyari, GM, Halawani, MA & Mirza, AA 2021, 'Depression and anxiety among medical students: a brief overview', Advances in Medical Education and Practice , vol. 12, pp. 393-8.
Molodynski, A, Lewis, T, Kadhum, M, Farrell, SM, Lemtiri Chelieh, M, Falcao De Almeida, T, Masri, R, Kar, A, Volpe, U, Moir, F, Torales, J, Castaldelli- Maia, JM, Chau, SWH, Wilkes, C & Bhugra, D 2021, 'Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries', International Review of Psychiatry, vol. 33, no. 1-2, pp. 37-42.
Monrouxe, LV, Hockey, P, Khanna, P, Klinner, C, Mogensen, L, O'Mara, DA, Roach, A, Tobin, S & Davids, JA 2021, 'Senior medical students as assistants in medicine in COVID-19 crisis: a realist evaluation protocol', BMJ Open, vol. 11, no. 9, p. e045822.
Nair, B, Moonen-van Loon, JMW, Parvathy, M & van der Vleuten, CPM 2021, 'Composite reliability of workplace based assessment of international medical graduates', MedEdPublish (2016), vol. 10, p. 104.
NSW Health 2021, Assistant in Medicine Evaluation Report, NSW Health, viewed 30 April 2024.
Parvathy, MS, Parab, A, BK, RN, Matheson, C, Ingham, K & Gunning, L 2021, 'Longitudinal outcome of programmatic assessment of international medical graduates', Advances in Medical Education and Practice, vol. 12, pp. 1095-1100.
Rajapuram, N, Langness, S, Marshall, MR & Sammann, A 2020, 'Medical students in distress: The impact of gender, race, debt, and disability', PLoS One, vol. 15, no. 12, p. e0243250.
Rupasinghe, S, Majeed Omar, M & Berling, I 2023, 'Final year medical students as Assistants in Medicine in the emergency department: a pilot study', Emergency Medicine Australasia, vol. 35, no. 4, pp. 600-604.
Scicluna, HA, Grimm, MC, Jones, PD, Pilotto, LS & McNeil, HP 2014, 'Improving the transition from medical school to internship -evaluation of a preparation for internship course', BMC Medical Education, vol. 14, p. 23.
Thorne, L, Duffy, C & Young, E 2024, 'Doing 1,000 hours of unpaid work to graduate is the reality of "placement poverty" -and it's taking a toll on students', ABC News, 2 March 2024, viewed 14 May 2024, https://www. abc.net.au/news/2024-03-02/university-accord-unpaid-student-poverty- placements/103511408