Evaluating combined VR-based stress management and de-escalation training for mental health nurses
Murielle G Kluge  1,2*, Sian James3, Elizabeth Ditton
1,2*, Sian James3, Elizabeth Ditton  1,4, Brendon Knott1,5, Steven Maltby
1,4, Brendon Knott1,5, Steven Maltby  4, Caroline Kuhne
4, Caroline Kuhne  1,
Rosemary Gallagher3, Frederick R Walker
1,
Rosemary Gallagher3, Frederick R Walker  1,2
1,2
Abstract
Aim:This study aimed to assess the acceptability, suitability and training impact of a virtual reality (VR)-based stress-management training tool for mental health nurses in Australia.
Background: VR is increasingly being considered a platform suitable for providing training to healthcare professionals. Barriers for adoption include both practical challenges inherent to the technology as well as end-user perceptions.
Design: We undertook a pilot feasibility study within a large public training hospital in Australia, to assess the acceptability, suitability, and training impact of the VR-based stress-management training platform, Performance Edge (PE). The program was integrated into a pre-existing one-day emotional awareness and regulation workshop at the Gold Coast Hospital and Health Service (Queensland, Australia) in September 2023.
Methods: Observational and self-report data were collected during implementation of the workshop, which integrated five VR-delivered stress- management lessons. Study participants were workshop attendees (mental health nurses) and educators involved in workshop delivery.
Results: All participants completed the workshop without encountering technical issues or adverse events. Both educators and attendees provided consistently positive feedback on PE’s usability, suitability, and relevance for healthcare settings. Participants reported increased knowledge, understanding and confidence in stress-management skills immediately and at follow-up, three to six weeks after the workshop. Moreover, clinicians reported actively using stress-management skills more after the training.
Conclusions:The VR platform offered practical stress-management skills training, professionals. The use of VR technology in general was also perceived as particularly valuable for this training context, providing a safe and immersive environment. By demonstrating acceptability across a range of metrics, this study supports the feasibility of using VR-delivered stress-management interventions within a clinical workforce. This feasibility trial is an important stepping stone for the broader implementation of VR within healthcare education.
Keywords: virtual reality, workplace training, stress management, de-escalation, emotional awareness, emotional dysregulation, mental health nurses
- Centre for Advanced Training Systems, College of Health, Medicine & Wellbeing, The University of Newcastle, Newcastle, Australia
- School of Biomedical Sciences & Pharmacy, College of Health, Medicine & Wellbeing, The University of Newcastle, Newcastle, Australia
- Gold Coast Hospital and Health Services, Mental Health Education, Mental & Health Specialist Services, Southport, Australia
- Hunter Medical Research Institute, Newcastle, Australia
- Contextual Interventions, Newcastle, Australia
Corresponding Author: Professor Frederick R Walker, Director of the Centre for Advanced Training Systems, The University of Newcastle, Medical Sciences Building Rm 317, Callaghan NSW 2308, Australia [email protected]
INTRODUCTION
Mental health nurses and other healthcare professionals frequently encounter aggressive and violent behaviours in the workplace (Joyce et al., 2023; Spelten et al., 2020). Verbal de-escalation has proven to be an effective strategy in managing these situations (Leanne Cowin et al., 2003; Du et al., 2017; Nambiar et al., 2020; Vieta et al., 2017), prompting a focus on comprehensive staff training to develop these skills (Bosse et al., 2016; Lavelle et al., 2016). However, de-escalation techniques alone do not mitigate the psychological stress often caused by repeated exposure to workplace violence. This exposure is linked to adverse outcomes, including PTSD, burnout, anxiety, sleep disturbances and reduced resilience (Ding et al., 2023; Lanctôt & Guay, 2014; Shi et al., 2017). Consequently, there is growing interest in combining de-escalation training with stress-management skills.
In Australian public hospitals, the need for timely patient care under sustained demand poses challenges for the allocation of resources to staff training. While most hospitals have mandatory de-escalation training, few address stress-management strategies, despite evidence highlighting the importance of emotional regulation for the management of challenging events (L. Cowin et al., 2003; Dafny & Muller, 2022).
A part of the reason underlying the paucity of stress-management training within public hospitals is the fact that large-scale, in-person training programs can be logistically and financially challenging for hospitals (and district health services) that manage thousands of employees. To overcome similar challenges with scaled stress-management training, the Australian Defence Force (ADF), in collaboration with the authors of the present study (MK, BK, ED, FRW), adopted an innovative approach leveraging virtual reality (VR) technology (Kluge et al., 2021). This strategy involved ntegrating clinically validated stress-management skills into a VR-based delivery platform, Performance Edge (PE), enabling the dissemination of critical training in a cost-effective and flexible manner (Kluge et al., 2023; Kluge et al., 2021). When evaluated in the context of defence force personnel, PE participants reported high levels of engagement and skill improvement, and that PE was easy to use (Kluge et al., 2023; Kluge et al., 2021).
Despite its potential, relatively few studies have explored VR for nursing staff training (Bracq et al., 2019; Frenk et al., 2022), and none (that we could identify) have focused on stress management. Potential barriers to the adoption of VR-based training include the complexity of the technology, IT infrastructure requirements and content suitability for healthcare contexts.
Given these issues, the specific study aims were to assess:
- whether the platform itself, both the technology and content, is feasible for a healthcare audience and workplace setting
- whether the stress-management training provided supports the training objectives
- training impacts on the participants, regarding perceived learning.
METHODS
STUDY DESIGN AND SETTING
Mental health nurse educators at a Queensland health service identified the need to update de-escalation training to include knowledge about escalating events and their impact on the stress response. A VR-based training solution, PE, was chosen to deliver emotional self-regulation training. A descriptive survey and observational study evaluated PE’s suitability within a classroom-based Emotional Awareness and Regulation Training Workshop at Gold Coast Hospital & Health Services (GCHHS).
The de-escalation refresher workshop, including the PE VR stress-management training was offered to mental health clinical staff at GCHHS who had previously attended the Occupational Violence Prevention (OVP) Refresher, or the Trauma Informed Care (TIC) Workshop. Six VR workshops were conducted in September 2023 at Robina Hospital and Gold Coast University Hospital, involving 8–14 mental health clinicians per session. Training was delivered as a full-day training workshop (7–8 hours) and included all five PE modules. VR training modules were delivered sequentially throughout the day alongside face-to-face instruction, debriefing and real- world training components. Each VR module was 20–30 minutes in length and was interrupted by a minimum of 30 minutes of out-of-headset training activities, breaks or instruction. As such, the training workshop contained a total of 2.5 hours of in-headset time across a 7–8-hour training period.
STUDY PARTICIPANTS AND RECRUITMENT
Eligible participants included mental health nurses and other professionals who had previously attended de-escalation training. Participants were informed about the VR component and research activities before registration. Exclusion criteria included a history of severe cybersickness or motion sickness.
Attendees and educators were invited to participate in pre-and post-training surveys. A total of 62 staff attended the training workshop. Sixty attendees participated in the study component by providing pre-and post-survey feedback on the day, 33 completed the follow-up survey and all 5 Educators provided formal feedback after the training workshop. The study was conducted as a scheduled activity within the pre-existing workshop. There was clear communication that participation in the research study was completely voluntary and outside of their standard training requirements. Staff could attend the training but did not have to fill out the survey, which 2 staff decided not to do. Also, responses to individual survey questions were not mandatory, meaning there are cases where single responses to a question are missing. Late arrivals (over 30 minutes) were excluded due to the essential VR induction requirement.
ETHICAL CONSIDERATIONS
The Metro North Health Human Research Ethics Committee (HREC) approved the study (EC 00172) [Protocol: HREC/2023/MNHA/97678], co-registered at the University of Newcastle HREC (Ref. no: H-2023- 0394). Participants provided written, informed consent and were not compensated. The study was voluntary and separate from standard training. No identifiable data was retained or included in the analysis.
PE TRAINING AND INTEGRATION INTO DELIVERY
The PE software application features five training modules based on cognitive behavioural therapy (CBT) and acceptance and commitment therapy (ACT) principles, as detailed previously (Kluge et al., 2023; Kluge et al., 2021).
Each module focuses on specific skills or strategies and includes an introductory video, guided narration, personalised learning, practical training, user interactions, feedback, performance measures and opportunities for repetition (for further details see Table 1). The intent of the overall series of PE modules is to orientate the user to skills that can be used to self-regulate during stressful experiences as well as effectively manage thoughts, emotions and behaviours after a stressful event. For example, controlled breathing can be effectively used to regulate autonomic arousal during, as well as after, an event. Similarly, sensorimotor grounding can be used to inhibit rumination and cyclical thoughts and enable engagement with the present, either during or after a stressful event. Typically, each module begins with a brief introductory video that establishes the context and purpose of the module. The introduction is then followed by a series of six to eight exercises that are designed to allow scaffolded participatory learning.
As an example of an exercise, in Module 2 (controlled breathing), the participant is invited to engage in what they consider to be controlled breathing. They are also encouraged to take their headset off to do a series of squat exercises. They then re-enter the headset and are presented with traces of their breathing (respiratory rate waveforms) from each activity. The learning objective is to allow the trainee to understand how biofeedback data is presented and visualised, as well as to highlight how respiratory rate can be consciously and non-consciously altered.
The user interface is designed with a futuristic and generic aesthetic; the platform emphasises broad applicability. PE is delivered via Oculus Quest VR headsets (Meta, California) with handheld controllers and inside-out tracking; the system integrates biofeedback using a GoDirect respiratory belt (Vernier, USA) and custom software.
Workshops were full-day sessions led by mental health nurse educators and included all five PE modules. Educators first completed a 3-hour train-the-trainer session facilitated by the creative director and lead researcher, covering VR integration, navigation challenges and core module content. This session also focused on contextualising the modules within the broader workshop objectives. During the workshop, the PE modules were delivered sequentially, interspersed with face-to-face instruction, debriefing and real-world training activities. Each VR module lasted 20–30 minutes, with at least 30 minutes of out-of-headset time between sessions for other training activities, breaks and instructions. In total, participants spent 2.5 hours in VR over the course of the day.
MEASURES AND DATA COLLECTION
Observational data and self-report instruments
Qualitative data on the delivery format and VR training integration, adherence to planned timeframes, hardware charging and setup requirements were documented by the research team throughout. Self-report data were collected via three surveys for training participants and one for educators (Supplementary Table 1). Participants filled out pre-and post-training surveys before and directly after the one-day training workshop as well as a follow-up survey three to six weeks after the training workshop. Educators filled out a single post-delivery survey after the two-week training period. Constructs and domains within the surveys are informed by the Technology Acceptance Model and they contain questions modified from the VR Hardware Acceptance Model (Manis & Choi, 2019) and User Experience Questionnaire (Laugwitz et al., 2008). Study-specific questions were developed and adapted in consultation with the local mental health nurse educators and all study investigators. A full list of questions is provided in Supplementary Table 1. All surveys were distributed using a QR code and QuestionPro.
DATA ANALYSIS
Survey data from participants and educators were analysed separately using Prism V.8 (GraphPad, USA), with all responses included. Qualitative data from open-text survey questions were not formally analysed; instead, frequently mentioned points were identified and counted, with examples provided in the manuscript. Responses to 5-point Likert scales (1 = strongly disagree, 5 = strongly agree) are displayed as bar graphs (mean ± standard error of the mean [SEM] with individual data points) and reported as a percentage or a mean with a 95% confidence interval (CI). Data collected across time points were compared using two-tailed Wilcoxon sign rank tests, with significance set at p < 0.05 and 95% CI.
RESULTS
TRAINING POPULATION AND BACKGROUND
Workshop attendees were primarily mental health nurses (81.7%; n = 49/59), with others including occupational therapists (6.7%; n = 4), social workers (3.3%; n = 2), a psychologist (1.7%; n = 1) and other/ unspecified roles (5%; n = 3). Years employed in the local health service ranged from < 1 to > 30 years (mean: 6.9 years, SD ± 6.8; median: 4.5 years, IQR: 8). Time in current roles was > 6 years for 40% (n = 24/60), 3–6 years for 16.7% (n = 10), 1–3 years for 25% (n = 15), and < 1 year for 18.3% (n = 11). Limited VR experience was reported by participants (48%, n = 28/58, had never used VR; 5%, n = 3, were experienced) and educators (three had used VR once; two had no experience). At the workshop’s start, participants reported frequent exposure to challenging events (93.3% [n = 56/60] at least weekly, and 50% [n = 30] daily); and distressed consumers (95% [n = 57/60] at least weekly, and 55% [n = 33] daily) (Supplementary Figure 1). Regarding strategies for managing responses to distressed consumers, 22% (n = 13) used specific strategies often, 46% (n = 28) sometimes, 20% (n = 12) rarely, and 12% (n = 7) never.
PE SUITABILITY
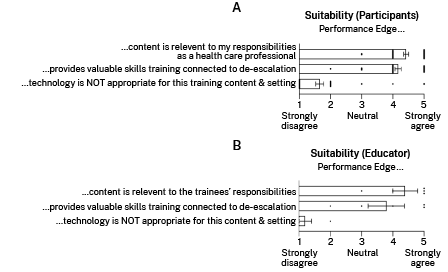
As PE was originally developed for a defence population, participants and educators were asked about its usefulness for healthcare professionals. Most participants (85%, 51/60) and educators (80%, 4/5) found the platform useful, with 15% of participants (n = 9) and one educator rating it ‘somewhat useful’ (Supplementary Figure 2A). Additionally, 93.3% of participants (56/60) and 80% of educators (4/5) agreed that PE training content is relevant to healthcare professionals in general (participants: mean = 4.4; 95% CI: 4.3–4.6; Figure 1).
Nearly all participants (59/60) found the skills taught in PE helpful for managing stress and emotional responses during or after escalating incidents (Supplementary Figure 2B). Four educators agreed PE supports de-escalation training, and one stated it was valuable for safety management training but not de-escalation. Similarly, 94.9% of participants (56/59) believed PE supported de-escalation training, while three found it valuable for other purposes. Most participants (96.7%, 58/60) indicated PE provided valuable skills for de-escalation (mean = 4.1; 95% CI: 4.0–4.4; Figure 1A), with three educators agreeing, one unsure, and one disagreeing (Figure 1B).
Most (90%) participants and all educators disagreed with the statement that VR technology was unsuitable for the workshop’s training content (participants: mean = 1.7; 95% CI: 1.4–1.9; Figure 1). All participants valued the provision of PE training to healthcare professionals, with 63% (37/59) finding it suitable in its current form, 31% (18/59) suggesting minor changes, and 7% (4/59) suggesting major changes.
Figure 1: PE suitability as assessed by mental health staff (A) and educators (B)
PERCEIVED TRAINING VALUE AND IMPACT
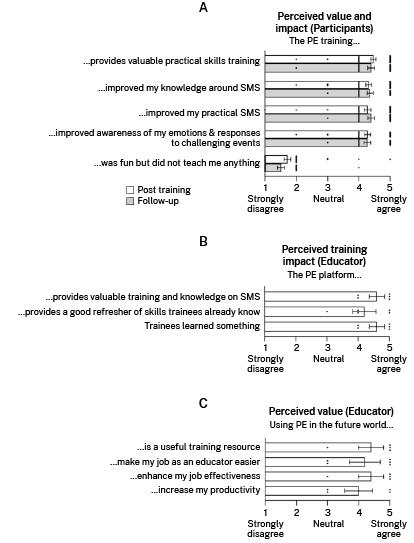
In the post-training survey, participants agreed that PE training provided valuable practical skills (mean = 4.5; 95% CI: 4.3–4.6), improved SMS knowledge (mean = 4.3; 95% CI: 4.1–4.5), improved practical stress management (mean = 4.3; 95% CI: 4.1–4.5), and awareness of emotions and stress responses (mean = 4.3; 95% CI: 4.1–4.5; Figure 2A). They disagreed with the statement that PE training lacked value (mean = 1.7; 95% CI: 1.5–1.9). These findings were consistent three to six weeks post-training (Figure 2A).
Educators affirmed PE as valuable for SMS training (2 = agree, 3 = strongly agree), a refresher for skills (2 = agree, 2 = strongly agree, 1 = neutral), and effective in teaching participants (2 = agree, 3 = strongly agree; Figure 2B). They described PE as a useful resource (1 = agree, 3 = strongly agree, 1 = neutral) that could simplify their roles (3 = strongly agree, 2 = neutral) and enhance productivity (1 = agree, 2 = strongly agree, 2 = neutral; Figure 2C).
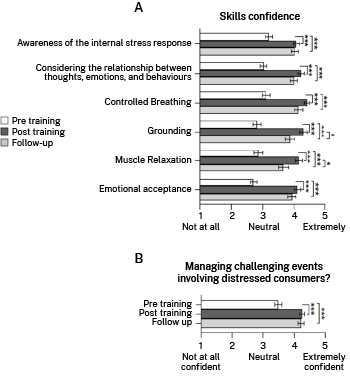
Skill confidence increased significantly post-training (Figure 3A). Mean differences (post–pre) in the Likert scores (all p < 0.0001) were:
- stress awareness = 0.88 (95% CI: 0.5–1.3)
- thoughts-emotions-behaviours = 1.2 (95% CI: 0.8–1.6)
- controlled breathing = 1.3 (95% CI: 0.9–1.7)
- progressive muscle relaxation (PMR) = 1.3 (95% CI: 0.9–1.7)
- grounding = 1.5 (95% CI: 1.0–1.9)
- emotional acceptance = 1.4 (95% CI: 1.0–1.8).
Skill confidence remained elevated at follow-up, compared to pre-training (Figure 3A), with slight declines for grounding (mean = 0.42, p = 0.043) and PMR (mean = 0.5, p = 0.020), though these still remained above the baseline pre-training levels.
Figure 2: Participant (A) and educator (B, C) perceptions of training impacts and value post-training and at 1 month follow-up
Participants reported greater confidence managing distressed consumers post-training (mean = 0.8; 95% CI: 0.5–1.0; p < 0.0001) and at follow-up (mean = 0.7; 95% CI: 0.4–1.1; p < 0.0001; Figure 3B).
After training, 97% (58/60) said they were likely to use the skills learned in the training (mean = 4.6; 95% CI: 4.5–4.8). At follow-up, 94% (31/33) had applied the skills, including controlled breathing (85%; 28/33), stress awareness (73%; 24/33), and emotional regulation (64%; 21/33). Grounding and PMR were used by fewer participants (45%; 15/33 and 39%; 13/33, respectively). Participants primarily used these skills to regulate emotions after encounters with distressed consumers (81%; 25/33); however, the skills were also used during (51%; 16/33) and before (48%; 15/33) these encounters.
Figure 3: Perceived confidence increases in SMS (A) and managing distressed consumers (B) after PE training (***P < 0.0001, *P < 0.05)
SPECIFIC FEEDBACK ON PE FORMAT AND CONTENT
Participants provided feedback on beneficial elements of the PE platform (Supplementary Table 2). In the post-training survey, key benefits included the training on emotional awareness and regulation (36%; n = 20) and the delivery format (22%; n = 12). Participants agreed that the VR technology facilitated an interactive and beneficial approach (18%; n = 10). At follow- up, the VR-based delivery remained a positive feature (18%; n = 6), but the content on controlled breathing was most valued (33%; n = 11). Emotional awareness, grounding techniques (18%; n = 6 each), real-world application (18%; n = 6), and customised feedback (15%; n = 5) were also highlighted features.
Sample quotes at follow-up:
‘[A beneficial component was] learning how to manage my own stress and emotions, which helps with helping my consumers.’
‘VR helped me use the techniques to a fuller extent than without VR. This gave me a state of mind to aim at when performing the techniques in everyday work life.’
Open-ended feedback with respect to improvements (Supplementary Table 3) included adding healthcare-specific scenarios (keeping in mind that the scenarios have been designed for adults, rather than to be occupationally specific), increased interactivity and puzzles, noise-cancelling earphones, and better image quality.
Sample quotes at follow-up regarding improvements:
‘Perhaps more mental health-specific scenarios could tailor this for staff.’
‘Better graphics and more comfortable seating for frequent training.’
Educators identified the immersive, safe and interactive environment, along with the practical skills focus, as the most beneficial aspects. The ability to reflect on one’s stress response privately, without judgement, was valued. Some educators reported attitude changes, with one stating:
‘Initially, I couldn’t see how VR would benefit healthcare professionals. However, after completing all five modules and seeing positive feedback, I now recognise its relevance to clinical practice.’
PE FEASIBILITY AND USABILITY
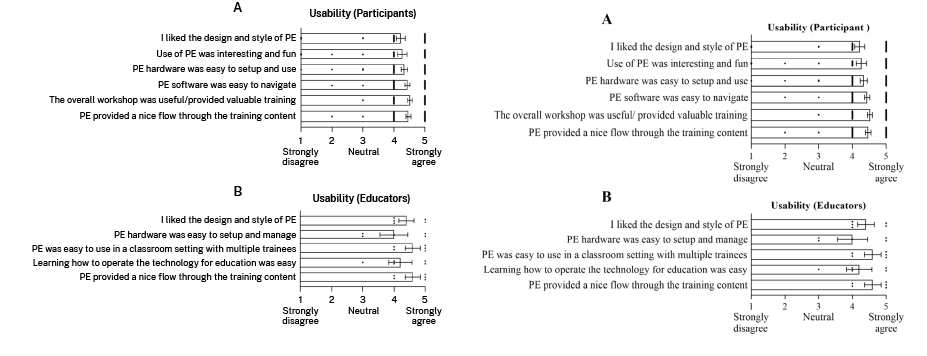
PE integration into the workshop was seamless, with room setup and pack-down taking 1.5 hours each. The management of 20 hardware units required storage and transport equipment (e.g., crates, trolley). All 62 participants completed the workshop without major technical issues. User questions concerning the interaction and interface were easily resolved on the spot with guidance from the educators. The only recurring technical issue related to the use of the respiratory belt, which required re-connection on multiple occasions and was specifically mentioned in post-training survey responses by two of the educators and three participants. Overall, 98% (58/59) of participants and all educators (5/5) were satisfied with the PE delivery (one participant responded ‘maybe’). Most participants found the hardware easy to set up (90%; 54/60; mean = 4.3, 95% CI: 4.1–4.5), the software easy to navigate (97%; 58/60; mean = 4.4, 95% CI: 4.3–4.6) and liked the design (87%; 52/60; mean = 4.3, 95% CI: 4.0–4.5). Additionally, 87% (52/60) found PE interesting and fun (mean = 4.3, 95% CI: 4.0–4.6; Figure 4A).
Educators agreed that participants enjoyed VR training and liked the platform design (Figure 4B). Three of the five found setup manageable, while two disagreed. All agreed PE was easy to use in group settings (2 = agreed, 3 = strongly agreed), and four felt prepared to deliver training, though one wanted more practice.
Figure 4: Mental health staff (A) and educator (B) perceptions of the usability of PE as a training resource
Participants rated the workshop as useful (96.7%; 58/60; mean = 4.5, 95% CI: 4.4–4.7) and felt VR ensured smooth content flow (96.7%; 58/60; mean = 4.5, 95% CI: 4.3–4.6). Follow-up surveys confirmed this, with 97% (32/33; mean = 4.4, 95% CI: 4.2–4.6) finding the workshop useful and 94% (31/33; mean = 4.3, 95% CI: 4.1–4.6) agreeing it was well-paced. Cybersickness symptoms were minimal. Most participants (83.3%; 50/60) reported no issues, while 16.7% (10/60) experienced mild effects such as heavy head (n = 2), cheek pressure (n = 3), eyestrain (n = 2), or mild disorientation (n = 2). Three participants and one educator reported mild nausea.
DISCUSSION
This pilot study evaluated the integration of a VR-delivered stress-management training tool into a pre-existing one-day de-escalation workshop for mental health nurses in a public hospital setting. The aim was to assess the feasibility and acceptability of delivering SMS training via VR to address the specific occupational challenges of mental health nurses. Both educators and clinical staff strongly endorsed the VR-based training, aligning with de-escalation objectives. Results showed increased understanding, skill use, and confidence in stress management, demonstrating real-world training transfer over three to six weeks. The platform’s content, delivery, and VR technology were highly valued in the healthcare setting.
This study also examined end-user acceptance, an often-overlooked aspect with regard to implementing new training systems (Granić & Marangunić, 2019). This was particularly important given that the platform had only been evaluated previously in defence populations. Findings confirmed the subject matter, delivery style, and VR technology were relevant to mental health nurses, offering an immersive, private environment for practice. The PE platform was regarded as a valuable tool for stress management and emotional awareness training by both participants and educators.
Immersive technologies like VR can improve healthcare education by providing safe, accessible training (Kluge et al., 2023; Kyaw et al., 2019). However, institutional and time constraints pose integration challenges (Sarre et al., 2018). This study demonstrated the feasibility of integrating PE into existing training activities (Moore et al., 2022; Weech et al., 2019). The train-the-trainer model enabled effective implementation, supporting feasibility, safety, and acceptance of VR in healthcare.
Training impacts included enhanced stress-management knowledge, practical skills confidence, and improved ability to handle challenging scenarios, addressing the theory-practice gap (Greenway et al., 2019). Research supports stress-management training as beneficial for the wellbeing of healthcare professionals (Alkhawaldeh et al., 2020; Babanataj et al., 2019; Chesak et al., 2019; Frenk et al., 2022; Nguyen et al., 2023; Sailaxmi & Lalitha, 2015; Till et al., 2024)
With respect to resourcing, the Performance Training VR package was developed with funding provided by the ADF 2018-2022. This funding was provided via the Capability Technology Demonstrator Scheme. Hardware (headsets and respiratory belts) and software, used in the project, were provided to mental health nurses at no cost. For context, ‘off the shelf’ VR headsets from electronics suppliers’ currently retail for between AUD400 and AUD800 (not including software). We have used the Oculus headset in the current project, but PE can run on most commonly available VR headsets. In addition to the PE program, we would also recommend the use of device management software, as it allows for simultaneous remote updating of the VR fleet.
Notable limitations of the current study include that it was conducted in a single Australian health district, limiting generalisability. However, the results provide evidence supporting VR training feasibility in Australian hospitals and suggest further investigation is warranted. Self-selection bias may have favoured participants with positive attitudes towards VR, and training impacts were assessed via self-report only. Future randomised controlled trials with standardised tools are necessary to validate these findings and evaluate long-term effects on mental health and workplace performance.
This pilot trial highlights VR’s potential in nursing education, particularly for objectives requiring a safe, immersive training environment like de-escalation. The mental health staff participants developed skills, knowledge and confidence in managing distressed consumers while protecting their own mental health. Positive feedback and high acceptance underscore the value of VR technology in nursing education.
Table 1: Study Activities and Training Schedule
Setting:
Full-day Training Workshop (8 am –4 pm)
Classroom of 8–15 mental health clinicians facilitated by two mental health nurse educators
Activity |
Duration |
Study information and consent |
10 min |
Pre-training survey (clinical staff) |
5 min |
Introduction presentation on how to set up, use and navigate the VR system |
20 min |
Performance Edge Module 1: Thoughts, Emotions and Behaviours An introduction to the training framework, outlining the value of noticing the distinction and connection between initial thoughts, emotions and behaviours in response to challenging events. |
30 min |
Out-of-headset de-brief and additional exercises |
30 min |
Performance Edge Module 2: Controlled Breathing Biofeedback-enabled practical training exercises on breath awareness and how to maintain a slow and steady breath to regulate the physiological stress response. |
25 min |
Out-of-headset de-brief and additional exercises |
20 min |
Morning Tea break |
15 min |
Performance Edge Module 3: Progressive Muscle Relaxation Practical guided exercise on noticing body tension, including body scan and progressive muscle relaxation. |
20 min |
Out-of-headset de-brief and additional exercises (and headset charging) |
20 min |
Lunch and headset charging |
30 min |
Performance Edge Module 4: Grounding Progressive exercises on how to direct and shift attention to auditory, visual, and sensory cues. |
30 min |
Out-of-headset de-brief and additional exercises |
30 min |
Performance Edge Module 5: Effectively Managing Emotions Practical exercises to notice, name and rate the intensity of emotions in response to different activities and environments, and to facilitate effective responding in the context of challenging emotions. |
20 min |
Out-of-headset de-brief and additional exercises |
20 min |
Post-training survey (clinical staff) |
10 min |
Afternoon tea |
15 min |
Out-of-headset de-brief: consolidation learning |
30 min |
THREE TO SIX WEEK GAP |
|
Follow-up survey (clinical staff) –online distribution |
10 min |
Acknowledgements:
We acknowledge the Australia Defence Force’s support for the development of PE VR via the Capability and Technology Demonstrator (CTD) Project (2018-2022). We acknowledge the incredible support of Jumpgate, and lead developer Lewis McLauchlan, for creation of the VR platform. We also thank SAPHI and Cameron Owen for contributions to the hardware and software integration utilised in the PE platform.
References
Alkhawaldeh, J. f. M., Soh, K. L., Mukhtar, F., Peng, O. C., Alkhawaldeh, H. M., Al-Amer, R., & Anshasi, H. A. (2020). Stress management training program for stress reduction and coping improvement in public health nurses: A randomized controlled trial. Journal of Advanced Nursing, 76(11), 3123-3135. https://doi.org/https://doi.org/10.1111/jan.14506
Babanataj, R., Mazdarani, S., Hesamzadeh, A., Gorji, M. H., & Cherati, J. Y. (2019). Resilience training: Effects on occupational stress and resilience of critical care nurses. International Journal of Nursing Practice, 25(1), e12697. https://doi.org/https://doi.org/10.1111/ijn.12697
Bosse, T., Gerritsen, C., & Man, J. d. (2016). An intelligent system for aggression de-escalation training Proceedings of the Twenty-second European Conference on Artificial Intelligence, The Hague, The Netherlands. https://doi.org/10.3233/978-1-61499-672-9-1805
Bracq, M. S., Michinov, E., Arnaldi, B., Caillaud, B., Gibaud, B., Gouranton, V., & Jannin, P. (2019). Learning procedural skills with a virtual reality simulator: An acceptability study. Nurse Educ Today, 79, 153-160. https://doi.org/10.1016/j.nedt.2019.05.026 Chesak, S. S., Cutshall, S. M., Bowe, C. L., Montanari, K. M., & Bhagra, A. (2019). Stress Management Interventions for Nurses: Critical Literature Review. Journal of Holistic Nursing, 37(3), 288-295. https://doi.org/10.1046/j.1440-0979.2003.00270.x Cowin, L., Davies, R., Estall, G., Berlin, T., Fitzgerald, M., & Hoot, S. (2003). De-escalating aggression and violence in the mental health setting. InternationalJournalofMentalHealthNursing,12(1),64-73. https://doi.org/ https://doi.org/10.1046/j.1440-0979.2003.00270.x
Cowin, L., Davies, R., Estall, G., Berlin, T.,
Fitzgerald, M., & Hoot, S. (2003). De-escalating aggression and violence in the mental
health setting. IntJMentHealthNurs,12(1),64-73. https://doi.org/10.1046/j.1440-0979.2003.00270.x
Dafny, H. A., &
Muller, A. (2022). Australian
nurses’ suggestions for the management of violence in the workplace: ‘The people who make the policy
are not the people on the floor’. Journal of Nursing Management, 30(6), 1454-1461. https://doi.org/https://doi.org/10.1111/jonm.13378
Ding, C., Li, L., Li, G., Li, X., Xie, L., & Duan, Z. (2023). Impact of workplace violence against psychological health among nurse staff from Yunnan-Myanmar Chinese border region: propensity score matching analysis. BMC Nursing, 22(1), 242. https://doi.org/10.1186/s12912-023-01402-w
Du, M., Wang, X., Yin, S., Shu, W., Hao, R., Zhao, S., Rao, H., Yeung, W. L., Jayaram, M. B., & Xia, J. (2017). De-escalation techniques for psychosis- induced aggression or agitation. Cochrane Database Syst Rev, 4(4), Cd009922. https://doi.org/10.1002/14651858.CD009922.pub2
Frenk, J., Chen, L. C., Chandran, L., Groff, E. O. H., King, R., Meleis, A., & Fineberg, H. V. (2022). Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet, 400(10362), 1539-1556. https://doi.org/10.1016/S0140-6736(22)02092-X
Granić, A., & Marangunić, N. (2019). Technology acceptance model in educational context: A systematic literature review. British Journal of Educational Technology, 50(5), 2572-2593. https://doi.org/https://doi. org/10.1111/bjet.12864
Greenway, K., Butt, G., & Walthall, H. (2019). What is a theory-practice gap? An exploration of the concept. Nurse Education in Practice, 34, 1-6. https:// doi.org/https://doi.org/10.1016/j.nepr.2018.10.005
Joyce, A., Pellatt, R., Ranse, J., Doumany, A., Hall, E., Sweeny, A., & Keijzers, G. (2023). Occupational violence in a tertiary emergency department: A retrospective descriptive study. Australasian Emergency Care, 26(4), 346- 351. https://doi.org/https://doi.org/10.1016/j.auec.2023.05.003
Kluge, M. G., Maltby, S., Kuhne, C., Walker, N., Bennett, N., Aidman, E., Nalivaiko, E., & Walker, F. R. (2023). Correction: Evaluation of a Virtual Reality Platform to Train Stress Management Skills for a Defense Workforce: Multisite, Mixed Methods Feasibility Study. J Med Internet Res, 25, e54504. https://doi.org/10.2196/54504
Kluge, M. G., Maltby, S., Walker, N., Bennett, N., Aidman, E., Nalivaiko, E., & Walker, F. R. (2021). Development of a modular stress management platform (Performance Edge VR) and a pilot efficacy trial of a bio-feedback enhanced training module for controlled breathing. PLOS ONE, 16(2), e0245068. https://doi.org/10.1371/journal.pone.0245068
Kyaw, B. M., Saxena, N., Posadzki, P., Vseteckova, J., Nikolaou, C. K., George, P. P., Divakar, U., Masiello, I., Kononowicz, A. A., Zary, N., & Tudor Car, L. (2019). Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration [Review]. J Med Internet Res, 21(1), e12959. https://doi.org/10.2196/12959
Lanctôt, N., & Guay, S. (2014). The aftermath of workplace violence among healthcare workers: A systematic literature review of the consequences. Aggression and Violent Behavior, 19(5), 492-501. https://doi.org/https://doi. org/10.1016/j.avb.2014.07.010
Laugwitz, B., Held, T., & Schrepp, M. (2008). Construction and Evaluation of a User Experience Questionnaire. In A. Holzinger, HCI and Usability for Education and Work Berlin, Heidelberg. Lavelle, M., Stewart, D., James, K., Richardson, M., Renwick, L., Brennan, G., & Bowers, L. (2016). Predictors of effective de-escalation in acute inpatient psychiatricsettings.JClinNurs,25(15-16),2180-2188. https://doi.org/10.1111/jocn.13239 Manis, K. T., & Choi, D. (2019). The virtual reality hardware acceptance model (VR-HAM): Extending and individuating the technology acceptance model (TAM) for virtual reality hardware. Journal of Business Research, 100, 503-513. https://doi.org/https://doi.org/10.1016/j.jbusres.2018.10.021
Moore, N., Ahmadpour, N., Brown, M., Poronnik, P., & Davids, J. (2022). Designing Virtual Reality–Based Conversational Agents to Train Clinicians in Verbal De-escalation Skills: Exploratory Usability Study. JMIR Serious Games, 10(3), e38669. https://doi.org/10.2196/38669
Nambiar, D., Pearce, J. W., Bray, J., Stephenson, M., Nehme, Z., Masters, S., Brink, D., Smith, K., Arendts, G., Fatovich, D., Bernard, S., Haskins, B., Grantham, H., & Cameron, P. (2020). Variations in the care of agitated patients in Australia and New Zealand ambulance services. Emergency Medicine Australasia, 32(3), 438-445. https://doi.org/https://doi. org/10.1111/1742-6723.13431
Nguyen, T., Pu, C., Waits, A., Tran, T. D., Ngo, T. H., Huynh, Q. T. V., & Huang, S.-L. (2023). Transforming stress program on medical students’ stress mindset and coping strategies: a quasi-experimental study. BMC Medical Education, 23(1), 587. https://doi.org/10.1186/s12909-023-04559-9
Sailaxmi, G., & Lalitha, K. (2015). Impact of a stress management program on stress perception of nurses working with psychiatric patients. Asian J Psychiatr, 14, 42-45. https://doi.org/10.1016/j.ajp.2015.01.002
Sarre, S., Maben, J., Aldus, C., Schneider, J., Wharrad, H., Nicholson, C., & Arthur, A. (2018). The challenges of training, support and assessment of healthcare support workers: A qualitative study of experiences in three English acute hospitals. International Journal of Nursing Studies, 79, 145-153. https://doi.org/https://doi.org/10.1016/j.ijnurstu.2017.11.010
Shi, L., Wang, L., Jia, X., Li, Z., Mu, H., Liu, X., Peng, B., Li, A., & Fan, L. (2017). Prevalence and correlates of symptoms of post-traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross-sectional study. BMJ Open, 7(7), e016810. https://doi.org/10.1136/bmjopen-2017-016810 Spelten, E., Thomas, B., O’Meara, P. F., Maguire, B. J., FitzGerald, D., & Begg, S. J. (2020). Organisational interventions for preventing and minimising aggression directed towards healthcare workers by patients and patient advocates. Cochrane Database Syst Rev, 4(4), CD012662. https://doi.org/10.1002/14651858.CD012662.pub2 Till, B., Hofhansl, A., & Niederkrotenthaler, T. (2024). Effects of the mental health promotion seminar ‘Coping with stress’ in the undergraduate medical curriculum of the Medical University of Vienna. BMC Medical Education, 24(1), 41. https://doi.org/10.1186/s12909-023-05019-0
Vieta, E., Garriga, M., Cardete, L., Bernardo, M., Lombraña, M., Blanch, J., Catalán, R., Vázquez, M., Soler, V., Ortuño, N., & Martínez-Arán, A. (2017). Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatry, 17(1), 328. https://doi.org/10.1186/s12888-017-1490-0
Weech, S., Kenny, S., & Barnett-Cowan, M. (2019). Presence and Cybersickness in Virtual Reality Are Negatively Related: A Review. Frontiers in psychology, 10, 158. https://doi.org/10.3389/fpsyg.2019.00158